The Burden of Schizophrenia
- Schizophrenia is one of the top 25 leading causes of disability worldwide.
- Individuals with schizophrenia have a life expectancy that is 10-25 years shorter than the general population.
- The health, social, and economic burdens of schizophrenia are immense for patients, families, caregivers, and society at large.
In this section
Societal and Economic Burdens
Despite being a disorder with relatively low prevalence, schizophrenia is ranked among the top 25 leading causes of disability1. Even with best practice treatment, outcomes are often suboptimal given the complexity of the disorder and its wide-ranging consequences.
Although there are considerable differences in the distribution of costs and service utilization for schizophrenia around the world, the global economic burden of schizophrenia is enormous. The main components of cost are associated with direct healthcare costs (eg, inpatient costs, outpatient costs, emergency department visits, prescription drugs), direct non-healthcare costs (eg, law enforcement, homeless shelters) and indirect costs (eg, unemployment, lost productivity, premature mortality, caregiver time). Recent examples of analyses conducted to estimate costs in schizophrenia include a systematic review of studies from 24 countries in 4 regions (Europe, US, Asia-Pacific, Africa) where the annual costs ranged from US $94 million to US $102 billion2. In an additional US study, the estimated cost of schizophrenia was $155.7 billion for 2013, with the largest contributors to excess costs associated with unemployment (38%), lost productivity (34%), and direct health care costs (24%)3. Indirect healthcare costs were the main drivers of excess cost in both of these analyses.
Acknowledging the Human Burden
In patients with schizophrenia, decline in mental function and social relationships over time can lead to social isolation, stigma, worse functional and cognitive impairment, reduced quality of life, and poor physical health, which creates burdens not only for individuals with schizophrenia, but for their caregivers and families alike4,5.
Patients
Many factors contribute to premature mortality in patients with schizophrenia. The average life expectancy of people with schizophrenia is reduced by 10-25 years compared with the general population6. Further, a retrospective US database analysis found that adults with schizophrenia were more than 3.5 times as likely to die during follow-up as adults in the general population7. The main factors associated with excess premature mortality in patients with schizophrenia are an unhealthy lifestyle, poor physical health, a 12-times increased risk of suicide, and side effects of antipsychotic drugs8,9. People with schizophrenia are not only more likely than others to have cardiovascular disease risk factors, including excess weight, smoking, high blood pressure, and metabolic syndrome, but they are less likely to receive preventative care10,11. Additionally, several second-generation antipsychotics are more likely to cause weight gain and subsequent metabolic syndrome12, which is associated with a 2- to 3-fold increase in cardiovascular mortality and a 2-fold increase in all-cause mortality13. Given that many causes of excess early mortality in schizophrenia are associated with preventable risk factors, key treatment goals for patients with schizophrenia should include good overall physical health, improved access to healthcare, and better screening practices14.
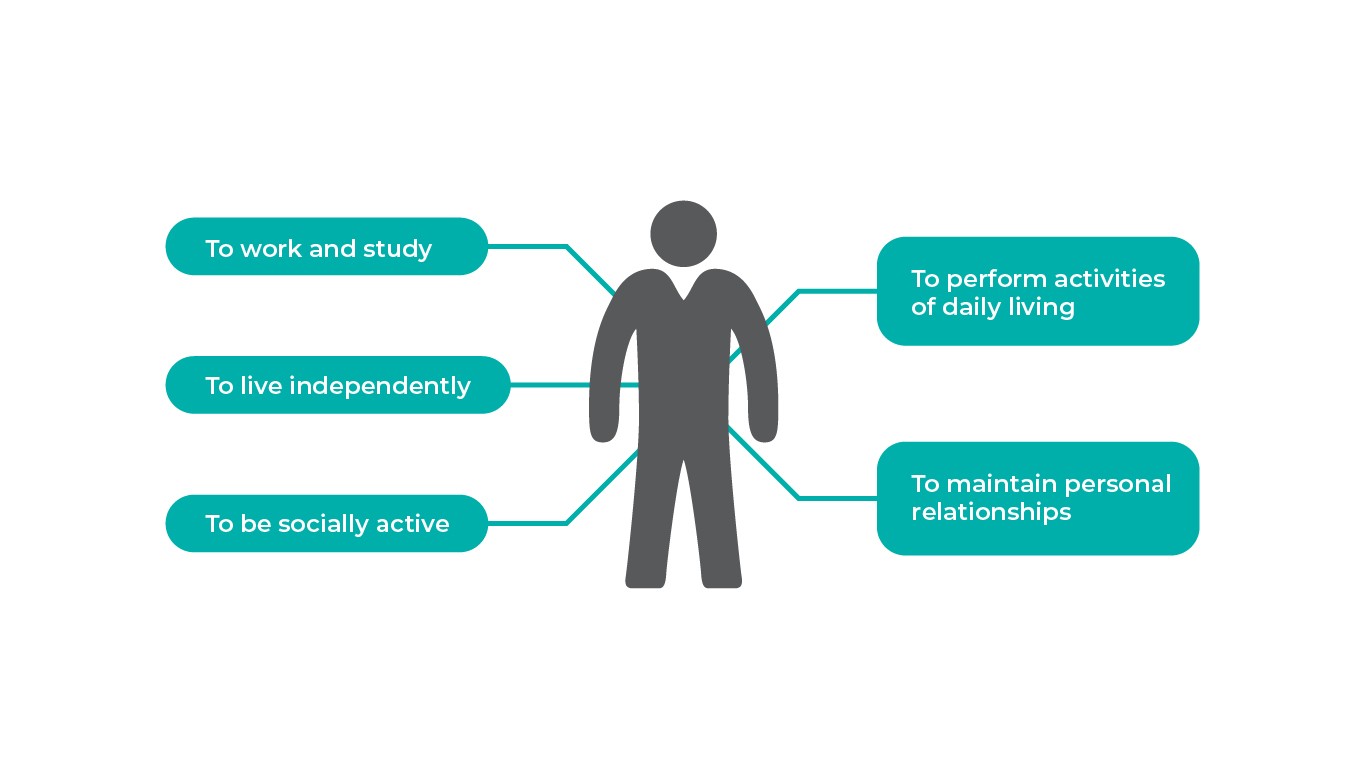
Schizophrenia is a highly heterogeneous disorder, with patient outcomes that can range from complete recovery to the need for comprehensive care. Unfortunately, complete recovery in schizophrenia is not the usual outcome15 and patients often experience impairments in social relationships, sustaining employment, and independent living16. Even after patients achieve remission from psychotic symptoms, deficits often persist because functional outcomes largely depend on the presence and severity of cognitive and negative symptoms, which are challenging to treat17. As may be expected, patients with schizophrenia have lower quality of life than the general population, with worse decrements associated with longer duration of illness, negative or depressive symptoms, medication side effects, and lack of family support. Among patients with schizophrenia, better quality of life is reported in younger people, women, married people, and individuals with a lower level of education. Treatment with antipsychotics that have a good tolerability profile and the addition of psychosocial treatments can also improve quality of life18,19.
Negative Symptoms Add to the Burden of Schizophrenia20–25
Negative symptoms are widely recognized as significant predictors of poor outcomes in schizophrenia. They carry a high burden of illness due to their pervasiveness, persistence, link to poor functional outcomes, increased costs due to higher healthcare utilization, and adverse influence on quality of life26,27.
Within the negative symptom domain, motivational deficits appear to be one of the most important predictors of functional impairment, with evidence further suggesting a potential interaction between negative symptoms and cognitive symptoms in regard to impaired function28. The limited number of effective treatment options for negative symptoms is a serious unmet medical need that increases the burden of illness in schizophrenia.
Caregivers
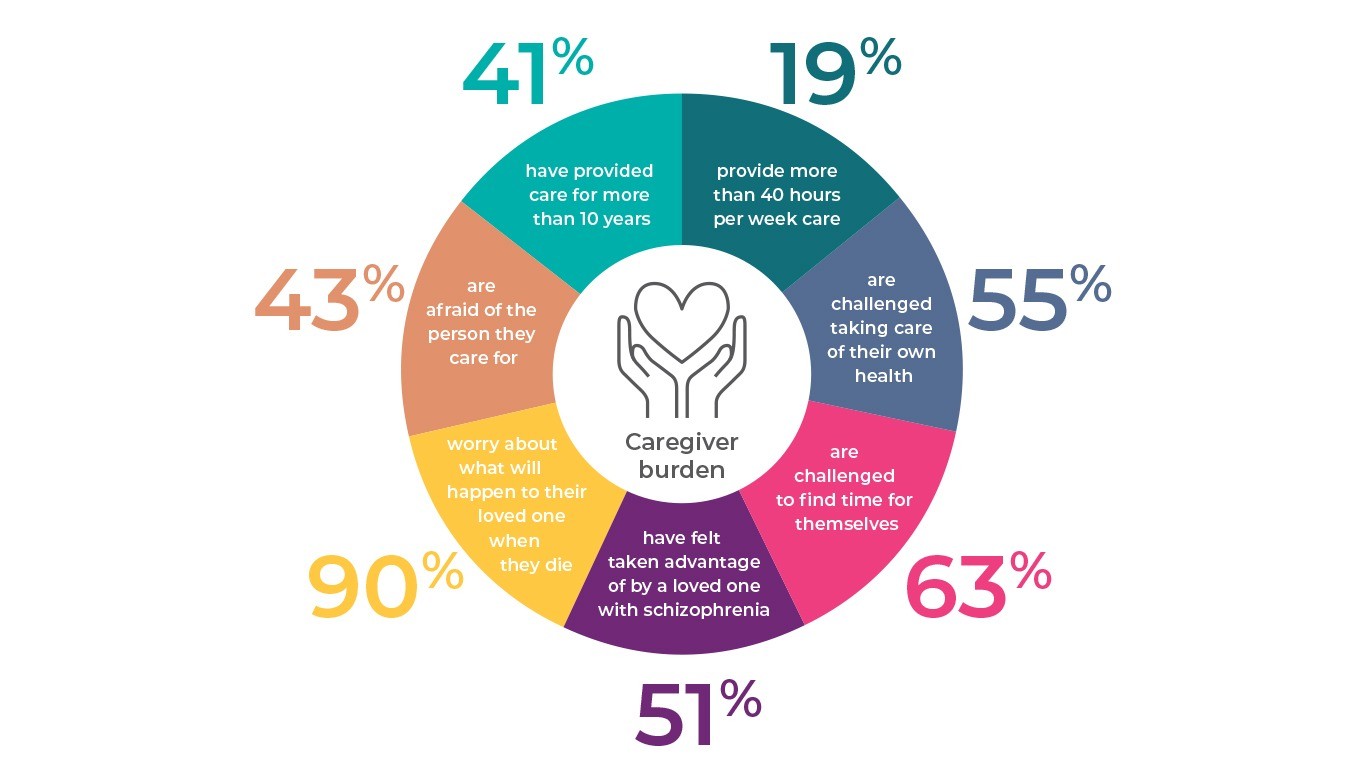
Patients with schizophrenia often require extensive help with personal care, medication management, and everyday activities4. Family members make up the bulk of the caregiver population for people living with schizophrenia. In a survey, 68% of caregivers were identified as parents, 12% were siblings, 7% were spouses or significant others, and 7% were the children or grandchildren of the person under their care29. Caregivers may be negatively affected by work overload at home, sleep disturbance, financial problems, less spare time, stigma, and social isolation4. Studies have shown that many caregivers experience significant cognitive, psychological (eg, anxiety, depression) social (eg, stigmatization, isolation), and financial burdens30-32. Caregivers’ work productivity and careers suffer when they have to leave their employment or reduce their hours to care for someone.
Reduced quality of life of caregivers in numbers32
As may be expected, symptom severity, level of patient disability, and hostility are associated with higher family burden33,34, but studies have been equivocal regarding the relationship between positive and negative symptoms and caregiver burden. While some studies have linked positive symptoms to greater family disruption and embarrassment, others have found that dealing with motivational issues requires more caregiver time and energy35-37.
References
- Vos, T. et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 390, 1211–1259 (2017).
- Chong, H. Y. et al. Global economic burden of schizophrenia: A systematic review. Neuropsychiatr. Dis. Treat. 12, 357–373 (2016).
- Cloutier, M. et al. The economic burden of schizophrenia in the United States in 2013. J. Clin. Psychiatry 77, 764–771 (2016).
- Millier, A. et al. Humanistic burden in schizophrenia: A literature review. J. Psychiatr. Res. 54, 85–93 (2014).
- Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Prim. 1, 1–23 (2015).
- Laursen, T. M., Nordentoft, M. & Mortensen, P. B. Excess Early Mortality in Schizophrenia. Annu. Rev. Clin. Psychol. 10, 425–448 (2014).
- Olfson, M., Gerhard, T., Huang, C., Crystal, S. & Stroup, T. S. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry 72, 1172–1181 (2015).
- Laursen, T. M., Munk-Olsen, T. & Vestergaard, M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr. Opin. Psychiatry 25, 83–88 (2012).
- Saha, S., Chant, D. & McGrath, J. A systematic review of mortality in schizophrenia: Is the differential mortality gap worsening over time? Arch. Gen. Psychiatry 64, 1123–1131 (2007).
- De Hert, M. et al. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC) Eur. Psychiatry 24, 412–424 (2009).
- Docherty, M., Stubbs, B. & Gaughran, F. Strategies to deal with comorbid physical illness in psychosis. Epidemiol. Psychiatr. Sci. 25, 197–204 (2016).
- Remington, G. Schizophrenia, antipsychotics, and the metabolic syndrome: Is there a silver lining? Am. J. Psychiatry 163, 1132–1134 (2006).
- Lakka, H. M. et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. J. Am. Med. Assoc. 288, 2709-2716 (2002).
- Suetani, S., Rosenbaum, S., Scott, J. G., Curtis, J. & Ward, P. B. Bridging the gap: What have we done and what more can we do to reduce the burden of avoidable death in people with psychotic illness? Epidemiol. Psychiatr. Sci. 25, 205–210 (2016).
- Jääskeläinen, E. et al. A systematic review and meta-analysis of recovery in schizophrenia. Schizophr. Bull. 39, 1296–1306 (2013).
- Harvey, P. D. Assessing disability in schizophrenia: tools and contributors. J. Clin. Psychiatry 75, e27 (2014).
- Reichenberg, A. et al. The course and correlates of everyday functioning in schizophrenia. Schizophr. Res. Cogn. 1, e47–e52 (2014).
- Bobes, J., García-Portilla, P., Sáiz, P. A., Bascarán, T. & Bousoño, M. Quality of life measures in schizophrenic patients. Dialogues Clin. Neurosci. 9, 215e-216e (2007).
- Bobes, J. & Garcia-Garcia, M. Quality of life in schizophrenia. in Quality of Life in Mental Disorders (eds. Katschnig, H., Freeman, H. & Sartorius, N.) 153–168 (John Wiley & Sons Ltd, 2005).
- Alonso, J. et al. Health-related quality of life (HRQL) and continuous antipsychotic treatment: 3-year results from the schizophrenia health outcomes (SOHO) study. Value Heal. 12, 536–543 (2009).
- Harvey, P. D. et al. Functional impairment in people with schizophrenia: Focus on employability and eligibility for disability compensation. Schizophr. Res. 140, 1–8 (2012).
- Rabinowitz, J. et al. Negative symptoms in schizophrenia – the remarkable impact of inclusion definitions in clinical trials and their consequences. Schizophr. Res. 150, 334–338 (2013).
- Kirkpatrick, B. & Buchanan, R. W. Anhedonia and the deficit syndrome of schizophrenia. Psychiatry Res. 31, 25–30 (1990).
- Fenton, W. S. & Mcglashan, T. H. Natural History of Schizophrenia Subtypes: II. Positive and Negative Symptoms and Long-term Course. Arch. Gen. Psychiatry 48, 978–986 (1991).
- Rabinowitz, J. et al. Negative symptoms have greater impact on functioning than positive symptoms in schizophrenia: Analysis of CATIE data. Schizophr. Res. 13, 147–150 (2012).
- Tandon, R. & Jibson, M. Negative symptoms of schizophrenia: How to treat them most effectively. Curr. Psychiatr. 1, 36–42 (2002).
- Sicras-Mainar, A., Maurino, J., Ruiz-Beato, E. & Navarro-Artieda, R. Impact of negative symptoms on healthcare resource utilization and associated costs in adult outpatients with schizophrenia: A population-based study. BMC Psychiatry 14, 225 (2014).
- Foussias, G., Agid, O., Fervaha, G. & Remington, G. Negative symptoms of schizophrenia: Clinical features, relevance to real world functioning and specificity versus other CNS disorders. Eur. Neuropsychopharmacol. 24, 693–709 (2014).
- The National Alliance on Mental Illness. Schizophrenia: Public Attitudes, Personal Needs Views from People Living with Schizophrenia, Caregivers, and the General Public. (2008).
- Chan, S. W. chi. Global Perspective of Burden of Family Caregivers for Persons With Schizophrenia. Arch. Psychiatr. Nurs. 25, 339–349 (2011).
- Gutiérrez-Maldonado, J., Caqueo-Urízar, A. & Kavanagh, D. J. Burden of care and general health in families of patients with schizophrenia. Soc. Psychiatry Psychiatr. Epidemiol. 40, 899–904 (2005).
- Hayes, L., Hawthorne, G., Farhall, J., O’Hanlon, B. & Harvey, C. Quality of Life and Social Isolation Among Caregivers of Adults with Schizophrenia: Policy and Outcomes. Community Ment. Health J. 51, 591–597 (2015).
- Awad, A. G. & Voruganti, L. N. P. The burden of schizophrenia on caregivers: A review. Pharmacoeconomics 26, 149–162 (2008).
- Magliano, L. et al. The impact of professional and social network support on the burden of families of patients with schizophrenia in Italy. Acta Psychiatr. Scand. 106, 291–298 (2002).
- Mantovani, L. M. et al. Family burden in schizophrenia: the influence of age of onset and negative symptoms. Trends Psychiatry Psychother. 38, 96–99 (2016).
- Grandón, P., Jenaro, C. & Lemos, S. Primary caregivers of schizophrenia outpatients: Burden and predictor variables. Psychiatry Res. 158, 335–343 (2008).
- Ochoa, S. et al. Do needs, symptoms or disability of outpatients with schizophrenia influence family burden? Soc. Psychiatry Psychiatr. Epidemiol. 43, 612–618 (2008).
Schizophrenia Research
Subjective and objective quality of life in schizophrenia.

Schizophrenia affects patients, caregivers and society. Often caregivers are the ones who suffer most.
Download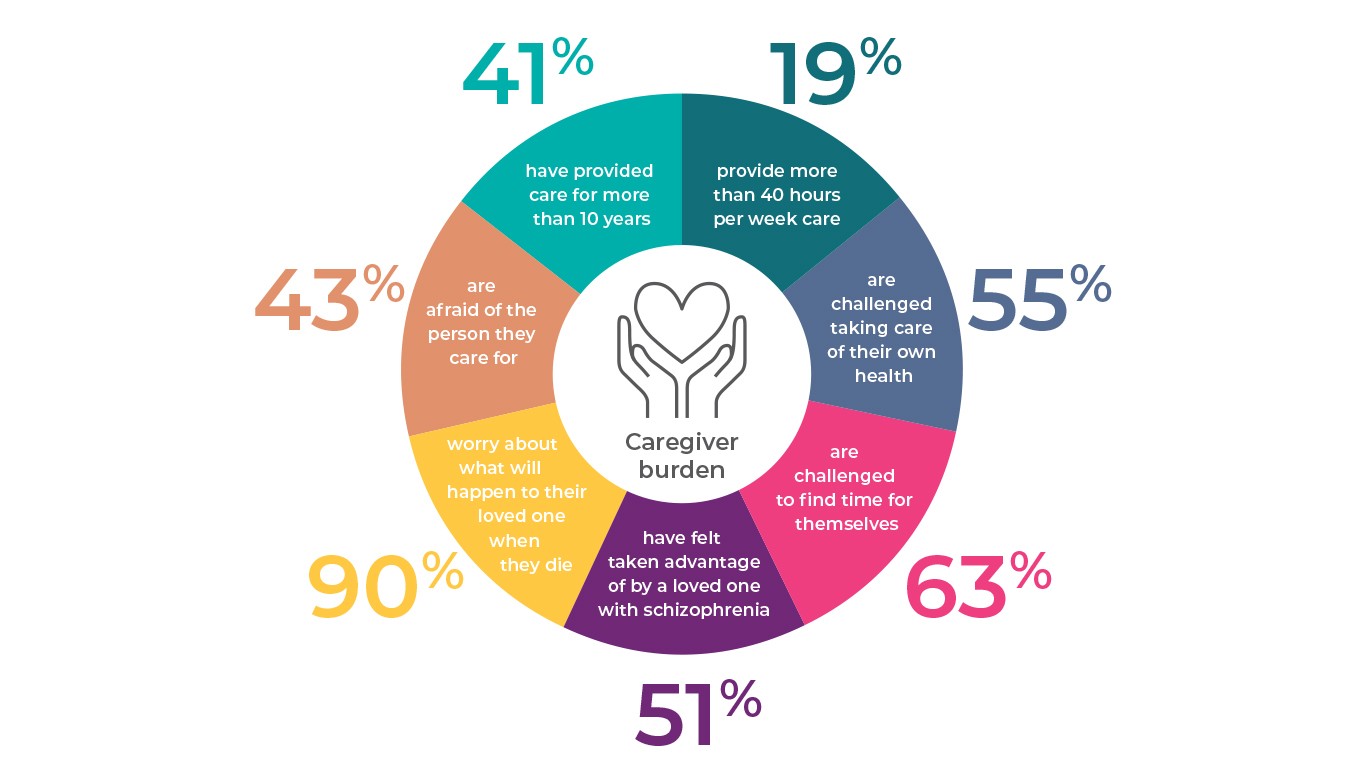
REAGILA AND DAILY FUNCTIONINGOUR PRODUCT AND DAILY FUNCTIONING
Negative symptom improvement must be accompanied by improved patient functioning in order for change to be considered clinically relevant in patients with schizNegative symptom improvement must be accompanied by improved patient functioning in order for change to be considered clinically relevant in patients with schiz
more…REAGILA IN ACUTE SCHIZOPHRENIAOUR PRODUCT IN ACUTE SCHIZOPHRENIA
Once the diagnosis of schizophrenia is made, clinicians, patients, and families have important treatment decisions to make. Although it seems intuitive to say tOnce the diagnosis of schizophrenia is made, clinicians, patients, and families have important treatment decisions to make. Although it seems intuitive to say t
more…