What is the Connection Between Inflammation and Schizophrenia?
In this section
Current Psychiatry Reports
Recent Advances in the Early Intervention in Schizophrenia: Future Direction from Preclinical Findings
Advances in the Early Intervention in Schizophrenia
Over the last few decades there has been increasing interest in early intervention and prevention of schizophrenia, a topic recently reviewed by Hashimoto and published in the Current Psychiatry Reports journal.1 Cognitive impairment is one of the key characteristics of the disease and studies have shown that this kind of impairment appears early, many years before the onset of psychosis and worsens post-psychosis onset.1 Therefore, early intervention and treatment of the cognitive symptoms may prevent progress to psychosis and offer a promising therapeutic approach.
Studies have looked at the features of early cognitive impairment and they have shown it is associated with a high inflammatory profile.1,2 In particular, positron emission tomography (PET) A technique that measures physiological function by looking at the blood flow, metabolism or neurotransmission, using radioactive injectable tracers3 studies have demonstrated high microglial activity The activity of the resident immune cells of the central nervous system (CNS), the microglia cells, measured by detection of secreted molecules2 in the brain of schizophrenia, which is an indicator of an inflammatory response.2 Moreover, researchers working with human cohorts and mouse models have shown that maternal immune activation (MIA), and thereby inflammation, during pregnancy causes long-term cognitive deficits in the offspring in adulthood.1 Therefore, inflammation is linked to the risk of developing psychosis later in life and this has led to the consideration of a range of anti-inflammatory medications for treatment of the disease.
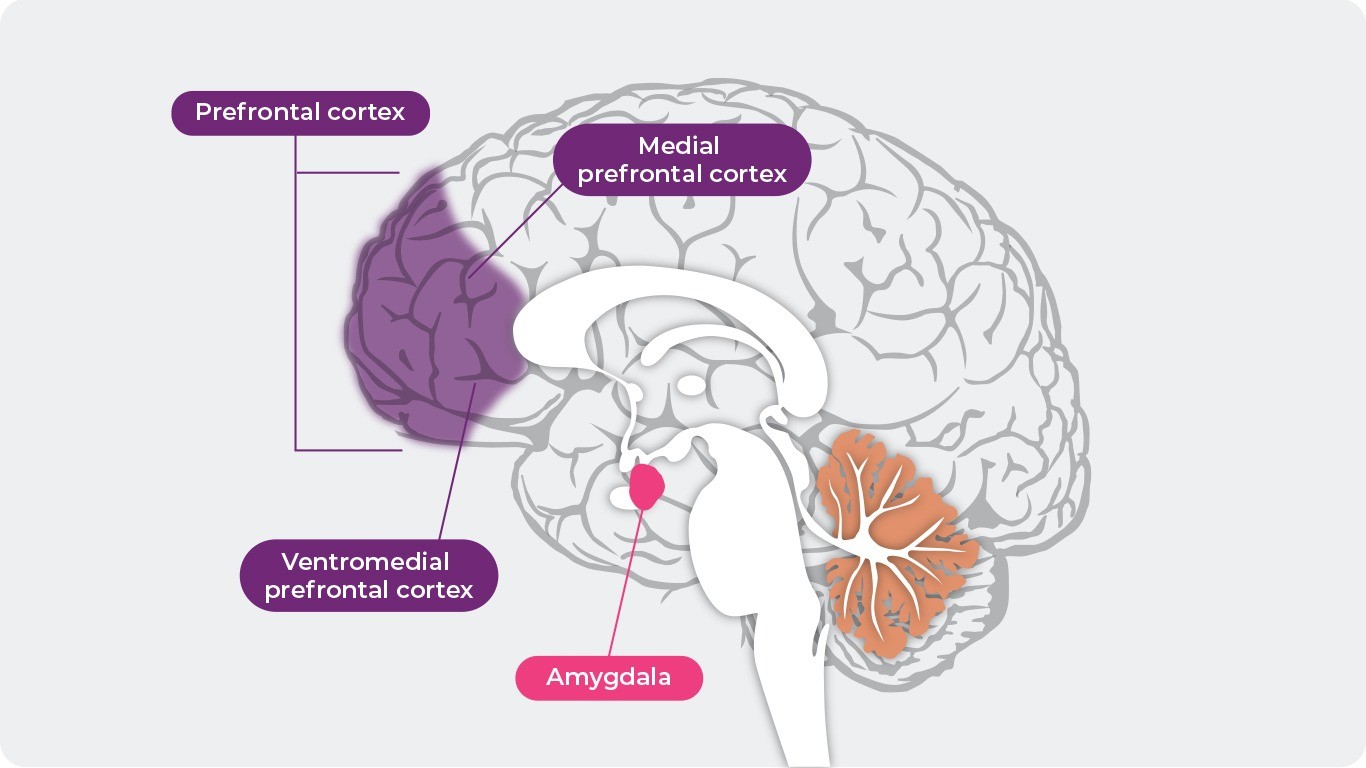
Recent advances in pre-clinical research have yielded positive findings related to anti-inflammatory treatment of adolescents at high risk of developing schizophrenia. Notably, some compounds might prevent the onset of behavioural abnormalities and parvalbumin A calcium-binding protein expressed in neurons of the CNS that is reduced in schizophrenia and therefore used as a marker to detect abnormal function4 immunoreactivity in the medial prefrontal cortex (Figure 1) of adult offspring after MIA.1 The table below summarises the potential candidate compounds for intervention, their mechanism of action, the animals they have been tested in preclinically and corresponding literature:1
Reference: Adapted from the National Institute of Mental Health
Potential candidates for intervention in psychosis
| Compound | Mechanism of Action | Key Findings |
| D-serine | NMDAR agonist | Supplementation during adolescence can lead to prevention of the onset of cognitive deficits in adult offspring after MIA5 |
| Rescue of schizophrenia-like behavioural abnormalities in adulthood caused by neonatal disruption of serine racemase6 | ||
| Sodium benzoate | DAO inhibitor | Efficacy as an adjunctive treatment in early Psychosis (study protocol for a randomized controlled trial)7 |
| 7,8-Dihydroxyflavone (DHF) | TrkB agonist | Treatment during juvenile and adolescent prodromal phase prevents onset of psychosis in adult offspring after MIA8 |
| Treatment from pregnancy to weaning prevents cognitive deficits in adult offspring after MIA9 | ||
| Prevents increase in levels of C1q in the prefrontal cortex of adult offspring after MIA10 | ||
| Sulforaphane (SFN) or its precursor glucoraphanin | Nrf2 agonist | Intake of sulforaphane-rich broccoli sprout extracts during juvenile and adolescence can prevent phencyclidine-induced cognitive deficits at adulthood11 |
| Dietary glucoraphanin prevents the onset of psychosis in the adult offspring after MIA12 | ||
| TPPU | Soluble epoxide hydrolase inhibitor | Soluble epoxide hydrolase has a key role in neurodevelopmental disorders of offspring after MIA13 |
MIA, maternal immune activation; DAO, D-amino acid oxidase; NMDAR, N-methyl-D-aspartate receptor
Reference: Adapted from Hashimoto. Current Psychiatry Reports. 21, 75 (2019)1
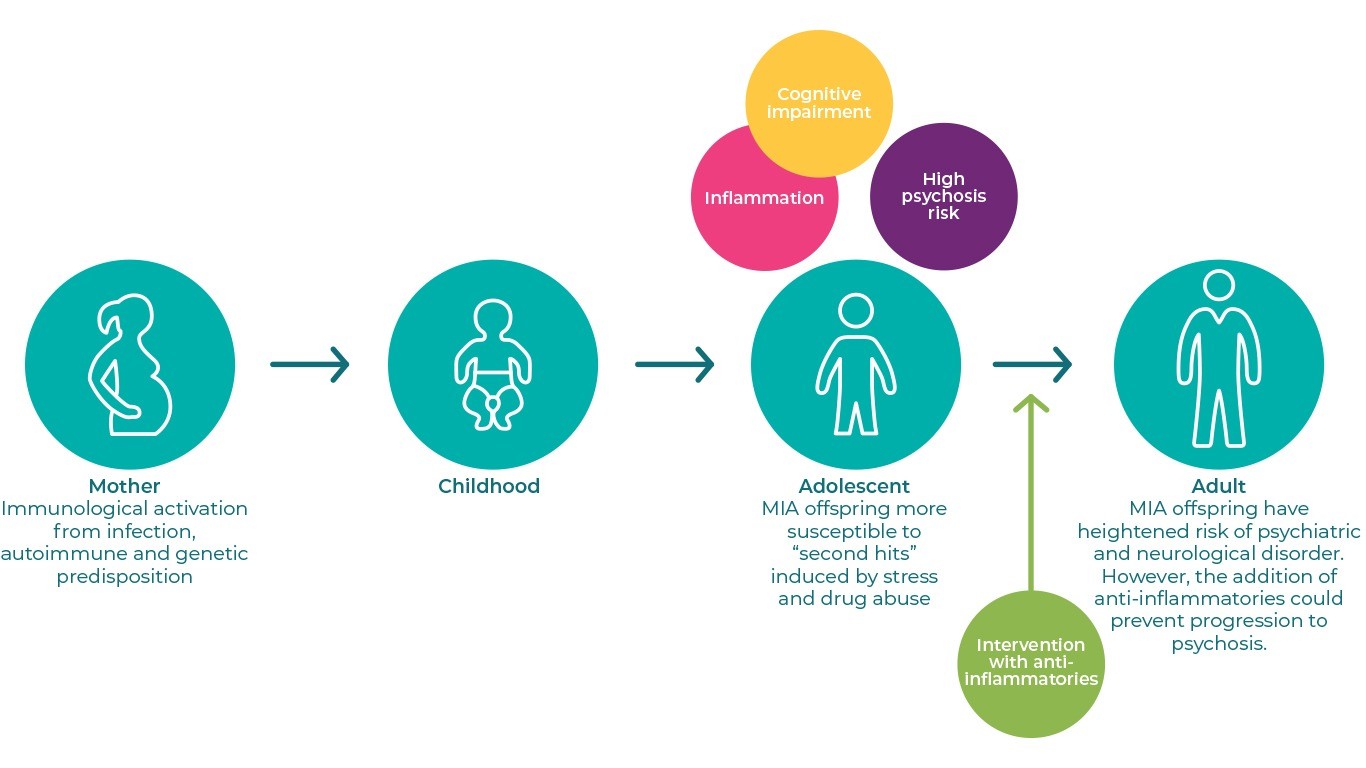
In conclusion, given the role of inflammation in prodromal cognitive impairment, early intervention using anti-inflammatory compounds seems to be a promising approach to prevent a subsequent transition to schizophrenia, as illustrated in the diagram below.14 The pre-clinical findings have set the grounds for the development of new treatments that will revolutionise clinical practice, by preventing progress of schizophrenia for first time, and alleviate the healthcare system from managing patients with a chronic life-long condition. An interesting longitudinal study showed that people at ultra-high risk of psychosis transitioned to psychosis at a rate of 9.6% after 6 months and 29.1% after 3 years, while the rates were lower for people at high risk.15 These results demonstrate that early intervention with safe anti-inflammatories could be beneficial for the latter group. In the future, it is necessary to conduct further randomized, double-blind, placebo-controlled study of the compounds mentioned above in young people with high risk for psychosis, in order to confirm this hypothesis.1 Furthermore, further research is required to establish accurate diagnostic methods for identification of cognitive symptoms at early stage.
Proposed mechanism of early intervention using anti-inflammatory compounds
Reference: Adapted from Estes and McAllister. Science. 353:772–7 (2016)14
References
- Hashimoto. Current Psychiatry Reports. 2019;21:75
- Bloomfield et al. Am J Psychiatry. 2016;173:44–52
- Berger et al. BMJ. 2003; 326
- Hayashida et al. Heliyon 5. 2019; e02037
- Fujita et al. Sci Rep. 2016;6:37261
- Hagiwara et al. PLoS One. 2013;8:e62438
- Ryan et al. Trials. 2017;18:165
- Han et al. Sci Rep. 2016;6:36087
- Han et al. Eur Arch Psychiatry Clin Neurosci. 2017;267:479–83
- Han et al. Clin Psychopharmacol Neurosci. 2017;15:64–7
- Shirai et al. PLoS One. 2015;10:e0127244
- Matsuura et al. Sci Rep. 2018;8:2158
- Ma et al. Proc Natl Acad Sci USA. 2019
- Estes and McAllister. Science. 2016;353:772–7
- Schultze-Lutter et al. Eur Psychiatry. 2015;30:405–16
CLOSER LOOK AT NEGATIVE SYMPTOMS!CLOSER LOOK AT NEGATIVE SYMPTOMS!
Negative symptoms are symptoms of loss or absence of normal function relating to motivation and interest, or emotional expression. Evidence does not support theNegative symptoms are symptoms of loss or absence of normal function relating to motivation and interest, or emotional expression. Evidence does not support the
more…REAGILA CONTROLS NEGATIVE SYMPTOMSOUR PRODUCT ON NEGATIVE SYMPTOMS
Negative symptoms of schizophrenia can occur as primary symptoms that are part of the underlying pathophysiology of schizophrenia or as secondary symptoms that Negative symptoms of schizophrenia can occur as primary symptoms that are part of the underlying pathophysiology of schizophrenia or as secondary symptoms that
more…