Selection of Schizophrenia Rating Scales
- Rating scales help with monitoring the severity of symptoms in schizophrenia. Up until the 1980s, researchers focused on the positive symptoms, but later on they switched to both positive and negative symptoms.1
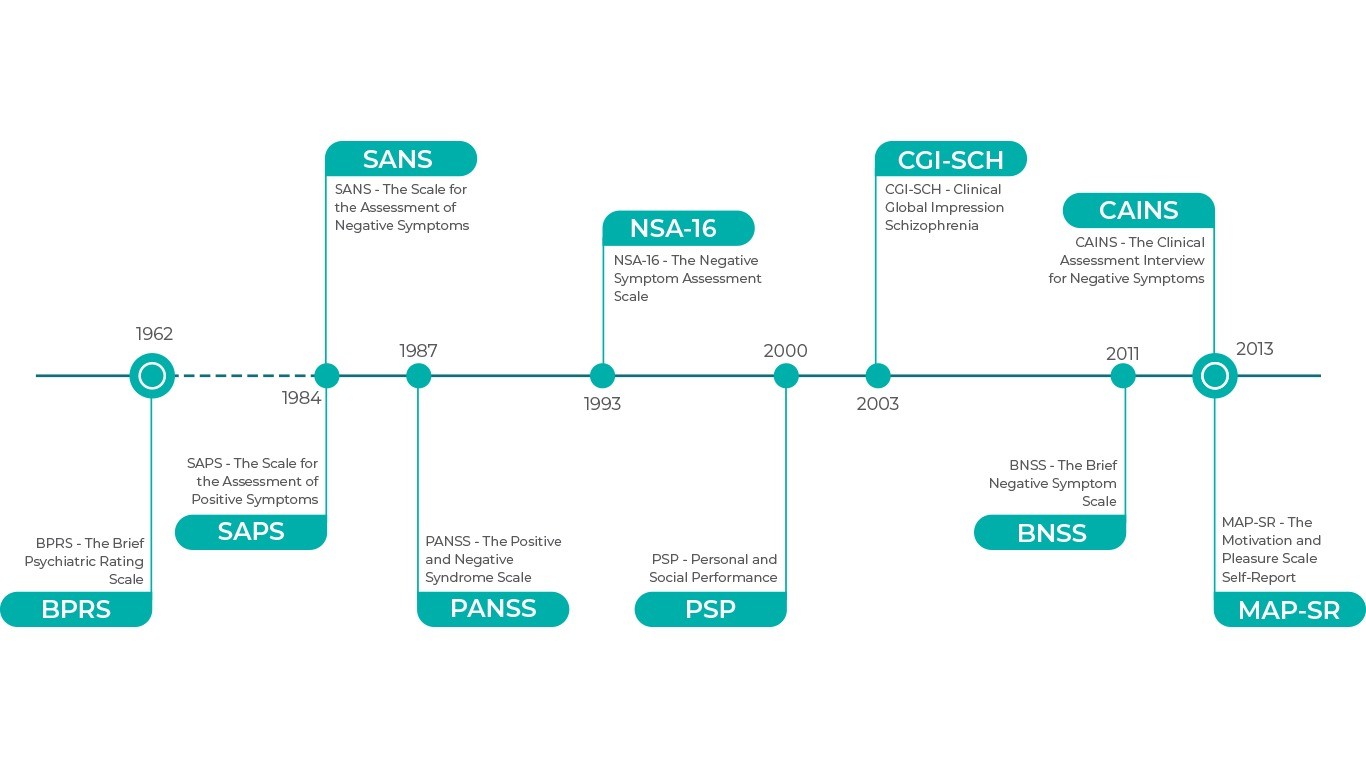
- Several psychometric scales have been developed and the most widely used in schizophrenia are presented below in chronological order.2
- Rating scales are used to define a series of items which quantify or place in rank order, the manifestations of a single variable, e.g. aggressiveness.3
- They are classified based on the user, the form of the items, their content and their function.3 Rating scales should only be considered as particular devices for recording information about a patient.3
In this section
Originally, the BPRS scale had 16 items, but later on two versions were developed, one with 18 items, and the BPRS-Extended (BPRS-E), with 24 items. The scale uses a seven-point Likert scale for item scoring.1
Commonly used factors include positive (thought disturbance, hostility–suspiciousness), negative (apathy, anergia, blunted affect, emotional withdrawal, motor retardation), agitation (animation, disorganization, activation) and mood symptoms (depression–anxiety, mood disturbances, affect).1
SANS uses 25 items and a 6-point scale to measure negative symptoms. The items are clearly defined and are organised into five domains: affective blunting, alogia, avolition/apathy, anhedonia/asociality and attention.1
This scale, together with the SAPS scale, have been criticized for their single focus on the negative or positive symptoms, which may be restricting those who use the scales to move beyond a dualistic model.1
The SAPS measures the severity of the positive symptoms on a 34 item, six-point scale, following a similar structure and format to SANS. The items used refer to hallucinations, delusions, bizarre behaviour and positive formal thought disorder, and are well-defined.1
The SANS and SAPS scales together have been criticized for their bi-dimensional relationship.1
PANSS is comprised of 30 items grouped into three subscales (positive, negative and general psychopathology) with scoring that ranges from 30 to 210 points.
Negative subscale: it assesses for blunted affect, emotional withdrawal, poor rapport, passive/apathetic social withdrawal, difficulty in abstract thinking, lack of spontaneity and flow of conversation and stereotyped thinking.
Positive subscale: it addresses delusions, conceptual disorganization, hallucinatory behaviour, excitement, grandiosity, suspiciousness and hostility.
General psychopathology subscale: it addresses somatic concern, anxiety, feelings of guilt, tension, mannerisms and posturing, depression, motor retardation, uncooperativeness, unusual thought content, disorientation, poor attention, lack of judgment and insight, disturbance of volition, poor impulse control, preoccupation and active social avoidance.1
This scale is known as the “gold standard”, however this title has been challenged. The main disadvantages of the PANSS scale are:1
Lack of sensitivity and specificity in predicting global cognitive functioning
Failure to differentiate between “depression, negative symptoms and extra-pyramidal side effects”
Its complexity, often leading to incorrect calculations
Factor analyses of the PANSS scale have identified five factors (Marder factors) that are aligned with the DSM-5 core criteria of positive symptoms, negative symptoms, disorganized thinking and the associated symptoms of hostility/excitement and depression/anxiety.8
This scale is a tool for evaluating negative symptoms of schizophrenia. The NSA-16 examines for the presence, severity, and range of negative symptoms associated with schizophrenia. The NSA-16 is a semi-structured 16 item interview, utilizing the five factors: communication, emotion/affect, social Involvement, motivation, retardation. Items are rated using a 6-point Likert scale where higher scores reflect greater impairment. Detailed anchoring criteria for the rating points are provided in the scale, along with a total score, sum of the scores on the 16-item scale, and a global negative symptom rating based on the global clinical impression of the patient’s negative symptoms.1
The main limitation of the NSA-16 is its high reliance on functioning or behaviors, even for experiential symptoms, such as reduced social drive, whose severity is measured by type and frequency of social interactions. This scale provides a focused assessment of negative symptoms, but it must be used in conjunction with a positive symptom rating scale.1
The PSP scale is a tool developed as social and personal functioning and it has two key characteristics: it measures four areas of functioning and its anchors only take into consideration the functioning of the individual, independently of symptomatology. The four areas of performance the PSP considers are:11
Socially useful activities, including work and study
Personal and social relationships
Self-care
Disturbing and aggressive behaviours
The clinician assesses the severity in each area (absent, mild, manifest, marked, severe or very severe), based on which a score is calculated. The final result is a single measurement from zero to 100% of functioning.11
Studies comparing the PSP scale to other scales indicate it is an adequate measure of social functioning in schizophrenia.11
This scale is used to assess the overall severity of schizophrenia and degree of change with regards to the positive, negative, depressive, cognitive and global symptoms, using a seven-point scale.1
Severity of illness: evaluation of disease state during the week previous to the assessment
Degree of change: change since the previous evaluation. Each category contains five different ratings
The disadvantages of the CGI-SCH scale are the lack of good interrater reliability and sensitivity to change.1
The BNSS, as well as the CAINS below, are scales that explore psychometric domains, including negative symptoms, different aspects of anhedonia and social interests, using 13 items to assess the negative symptoms.1 This scale is considered reliable with a concise and accessible format. However, it has been criticized for being restrictive, as it does not integrate other aspects of the patients’ social and cognitive functioning, and it’s based on the negative symptoms.1
The CAINS is an effective and validated tool that uses 13 items to assess negative symptoms in schizophrenia. It explores psychometric domains, including negative symptoms, different aspects of anhedonia, and interest in social relationships with others.1
CAINS is empirically developed and evaluates patients’ primary diagnosis on the basis of negative symptoms, with no integration of other aspects of the patients’ social and cognitive functioning. This scale is criticised for being too restrictive and not strongly related to depression, agitation, or positive symptoms.1
The self-administered scale MAP-SR consists of 15 items that assess patient motivation and pleasure. Items are grouped into four subscales:2
Social pleasure
Recreational or work pleasure
Feelings and motivations about close, caring relationships and
Motivation and effort to engage in activities
This scale uses a 5-point Likert scoring system where higher scores reflect less impairment.2
European Archives of Psychiatry and Clinical Neuroscience
Psychometric evaluation of the negative syndrome of schizophrenia
References
- Kumari et al. J Addict Res Ther. 2017, 8:3
- Garcia-Portilla MP. Eur Arch Psychiatry Clin Neurosci. 2015;265(7):559-66
- Editorial, Psychological Medicine. 1976, 6, 347—349
- Overall and Gorham. Psychological Reports. 1962;10:799-812
- Andreasen, University of Iowa, 1984
- Andreasen, University of Iowa, 1984
- Stanley et al. Schizophrenia Bulletin. 1987; 13(2):261–276
- Hopkins et al. Schizophrenia Bulletin. 2018; 44(3): 593–602
- Axelrod et al. Journal of Psychiatric Research. 1993; 27(3):253-258
- Morosini et al. Acta Psychiatr Scand. 2000; 101(4):323-329
- Menezes et al. J Bras Psiquiatr. 2012; 61(3):176-80
- Haro et al. Acta Psychiatr Scand Suppl. 2003;(416):16-23
- Kirkpatrick et al. Schizophrenia Bulletin. 2011; 37(2):300–305
- Kring et al. Am J Psychiatry. 2013;170:165–172
- Llerena et al. Compr Psychiatry. 2013; 54(5): 568–574
WHAT’S THE PSEUDOSPECIFICITY ISSUE?WHAT’S THE PSEUDOSPECIFICITY ISSUE?
Although cariprazine is the first and only antipsychotic to demonstrate efficacy against another antipsychotic in a large-scale trial specially designed to evalAlthough cariprazine is the first and only antipsychotic to demonstrate efficacy against another antipsychotic in a large-scale trial specially designed to eval
more…REAGILA IN ACUTE SCHIZOPHRENIAOUR PRODUCT IN ACUTE SCHIZOPHRENIA
Once the diagnosis of schizophrenia is made, clinicians, patients, and families have important treatment decisions to make. Although it seems intuitive to say tOnce the diagnosis of schizophrenia is made, clinicians, patients, and families have important treatment decisions to make. Although it seems intuitive to say t
more…