
Negative Symptoms: Getting to the Specifics
- Negative symptoms, a core symptom domain in schizophrenia, are described as a lessening or absence of normal behaviors and functions related to either motivation and interest, or emotional expression.
- Although patients may appear to be sad and withdrawn, negative symptoms are not depressive symptoms; instead, they represent a symptom domain in schizophrenia that is independent from depressive symptoms, positive symptoms, cognitive symptoms, and disorganization.
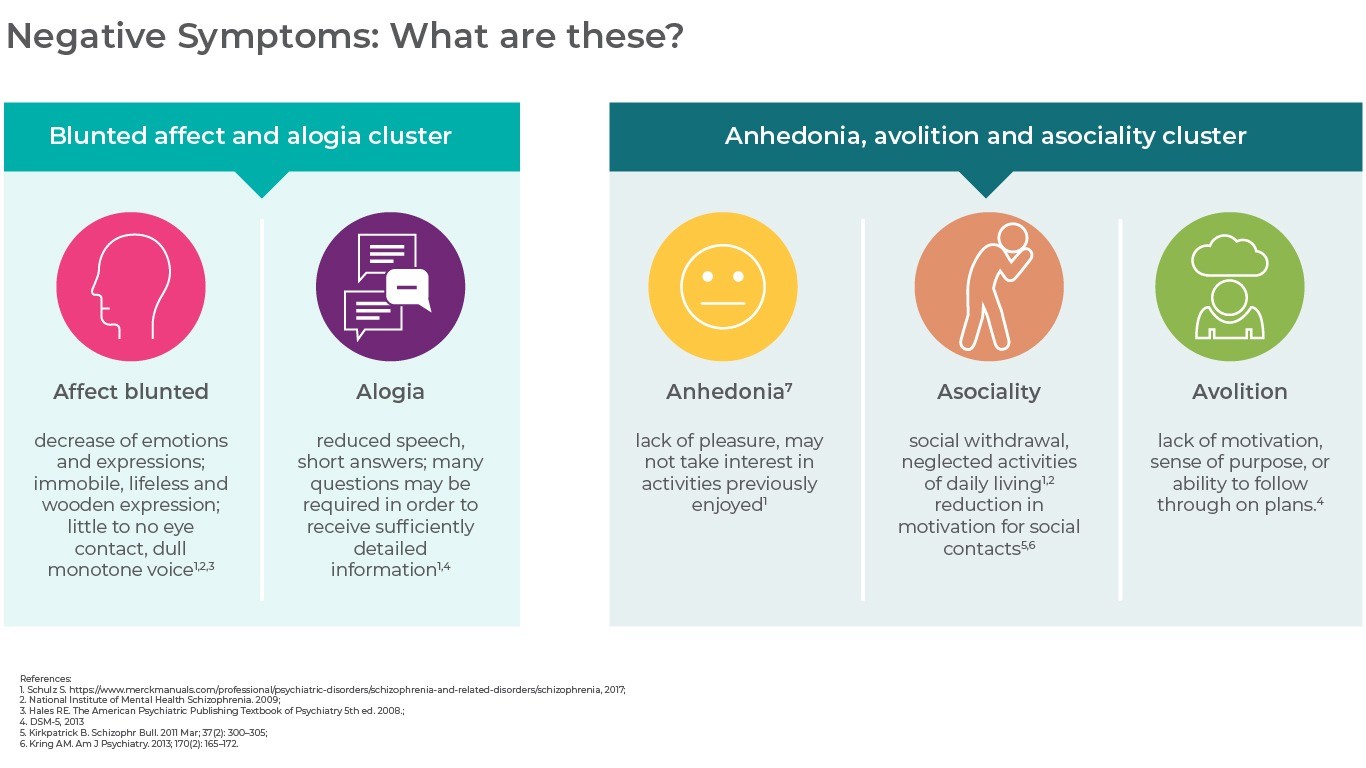
- Five constructs are recognized as key to the negative symptom domain: affect blunted, alogia, anhedonia, asociality, and avolition; these constructs are further categorized into clusters that differentiate the symptoms related to diminished expression (affect blunted and alogia) and reduced motivation and pleasure (anhedonia, asociality, and avolition).
In this section
A Core Domain of Schizophrenia
Negative symptoms are symptoms of loss or absence of normal function relating to motivation and interest, or emotional expression. Evidence does not support the idea of a common pathophysiology for the origin of both negative and positive symptoms and studies indicate that negative symptoms are independent from positive symptoms, cognitive dysfunctions, disorganization, and depression1,2.
Negative symptoms can cause significant deficiencies in motivation, affect, communication, and functioning3. These fundamental deficits have been recognized as an important aspect of schizophrenia pathology since the disorder was first described by Eugene Bleuler, in 1950: “An indifference to everything – to friends and relations, to vocation or enjoyment, to duties or rights, to good fortune or bad… expressionless faces, hunched-up, the image of indifference… The capacity for work, for caring for themselves diminishes…They no longer have the urge to do anything either of their own initiative or at the bidding of another…”4
Although negative symptoms may be challenging to recognize, especially if they are mild, they are more than just sadness5,6.
Key Negative Symptom Constructs: The 5 A’s
Blunted affect, alogia, anhedonia, asociality, and avolition are the 5 key constructs included in the negative symptom domain7:
Diminished Emotional Expression
(what you observe from the outside)
Affect blunted refers to a decrease in facial, vocal and gesture expressions, and is an overall diminished expression of emotion. In terms of vocal expressions, studies have shown that patients with schizophrenia have less accurate spontaneous and voluntary vocal emotions (reduced changes in the volume, speed and pitch of speech) than healthy subjects. In terms of expressive deficits involving facial expressions and gestures, an overall reduction in the patients’ nonverbal behavior has been reported. Expressive gestures, including those made with hands, arms, shoulders, face and head are important parts of human communication and social interaction that help a better understanding7.


Alogia, a reduction in the quantity of speech, is a general lack of additional, unprompted content which is usually observed in normal speech. It is evaluated during the clinical interview, and examines how much spontaneous speech production the patient has or whether he/she only gives short, monosyllable answers and does not elaborate on any topic on his/her own. A meta-analysis of studies has shown that patients with schizophrenia have a large reduction in this aspect of speech compared to healthy controls. Alogia in this context does not refer to impoverished content of speech, where a patient might produce many words and long sentences, but with little information7.


Reduced Motivation and Pleasure
(what the patient feels from the inside)
Asociality is defined as a reduction in social initiative to form close relationships with others. It is a reduction in the desire or motivation for social contacts, rather than just a behavioral aspect of not having social interactions, which can be secondary to factors such as delusions and hallucinations (fear of getting harmed by others), suspiciousness or depressed mood or lack of opportunities to establish and maintain social relationships (environmental deprivation)7.


Anhedonia, i.e. the diminished capacity to experience pleasant emotions, has traditionally been regarded as a core feature of both depression and schizophrenia.
Anhedonia appears to have 2 distinct attributes in schizophrenia—consummatory anhedonia (the inability to experience pleasure during an activity), which remains relatively intact in individuals with schizophrenia, and anticipatory anhedonia (the inability to anticipate future pleasure). Anticipatory anhedonia is a characteristic feature of negative symptoms that produces an inability to anticipate reward and reduces a patient’s motivation to seek out pleasant experiences7,8. Studies have shown that patients with schizophrenia do not differ from healthy controls in their subjective reactions to emotionally charged stimuli (so in consummatory anhedonia) as they do in anticipatory anhedonia. The mechanisms underlying these deficits may be partly explained by aspects of motivation and reward anticipation or effort valuation and cognitive functioning i.e. impaired episodic memory interfering with subject’s ability to recall previous pleasant experiences7.


Avolition is a reduced initiation and persistence of goal-directed activity, which results in a reduction of engagement in activities relevant to work, school, everyday life and hobbies. There is no agreement on the degree of overlap between the terms avolition, decreased drive, amotivation and apathy, and they are often considered interchangeable. Avolition in the framework of schizophrenia is characterized by a reduction of interest to initiate or participate in activities and is not accompanied by feelings of guilt, sadness or insufficiency in doing so. The patients usually neither miss nor feel the need to initiate or follow through with activities. In contrast, reduction in initiation and goal-oriented activity can be secondary to factors such as depressed mood (avolition is accompanied by feelings of sadness or guilt) or lack of opportunities (patient may have little or no opportunity for participating in activities). Impairment in reward functioning is hypothesized as the core aspect in avolition7.


According to studies, social amotivation is the most common negative symptom, followed by diminished expression and alogia9–11.
Two Stable Negative Symptom Factors
There are several clusters of negative symptoms described in the literature, with evidence emerging in support of models generally consisting of 2 to 5 factors, of which the most stable and replicated factor models include the 2 factors of12:
diminished emotional expression (affect blunted, alogia) and
reduced motivation and pleasure (anhedonia, asociality, avolition).
These factors may be associated with different underlying neurobiological abnormalities and psychosocial outcomes13. For example, the diminished expression factor may have a stronger association with nonsocial and neuropsychological function14, while the avolition/apathy factor is theorized to have a direct impact on functional outcomes in schizophrenia3.
Negative Symptom Dimensions
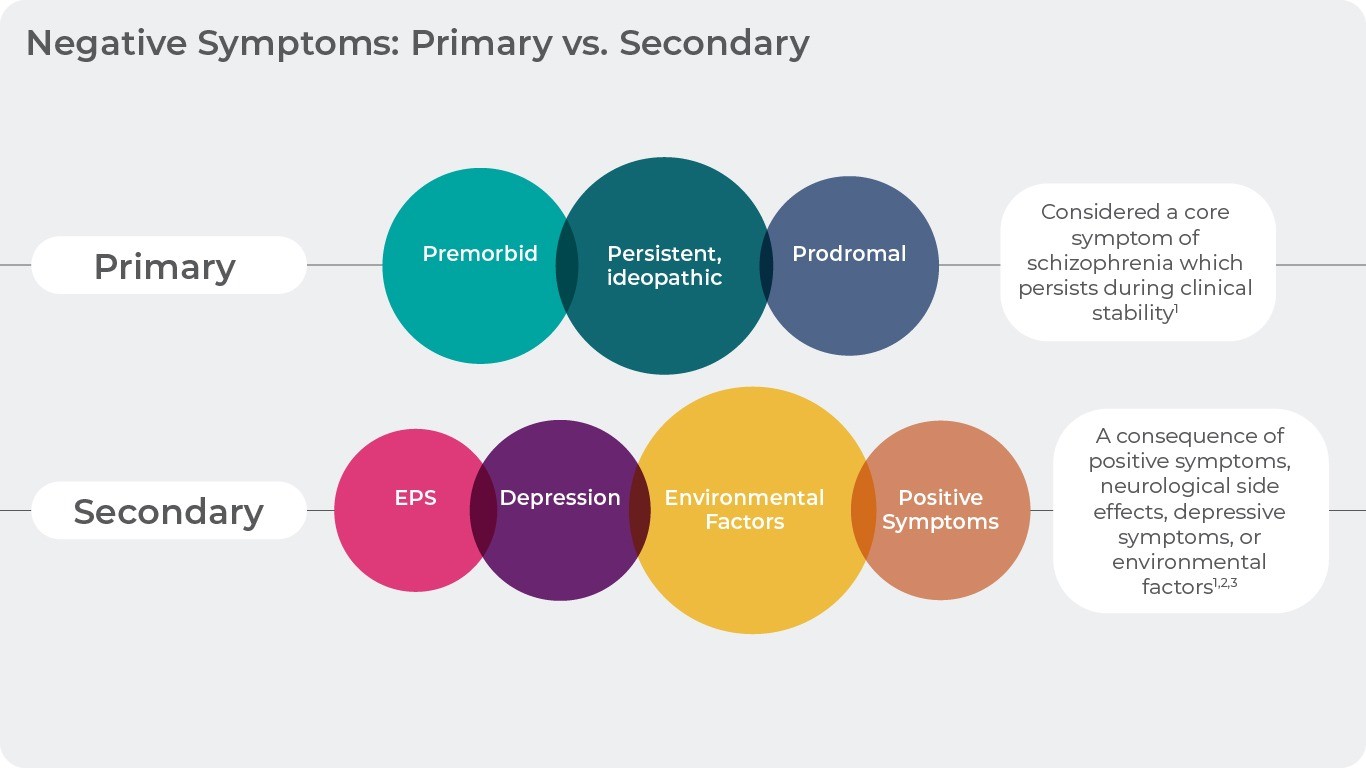
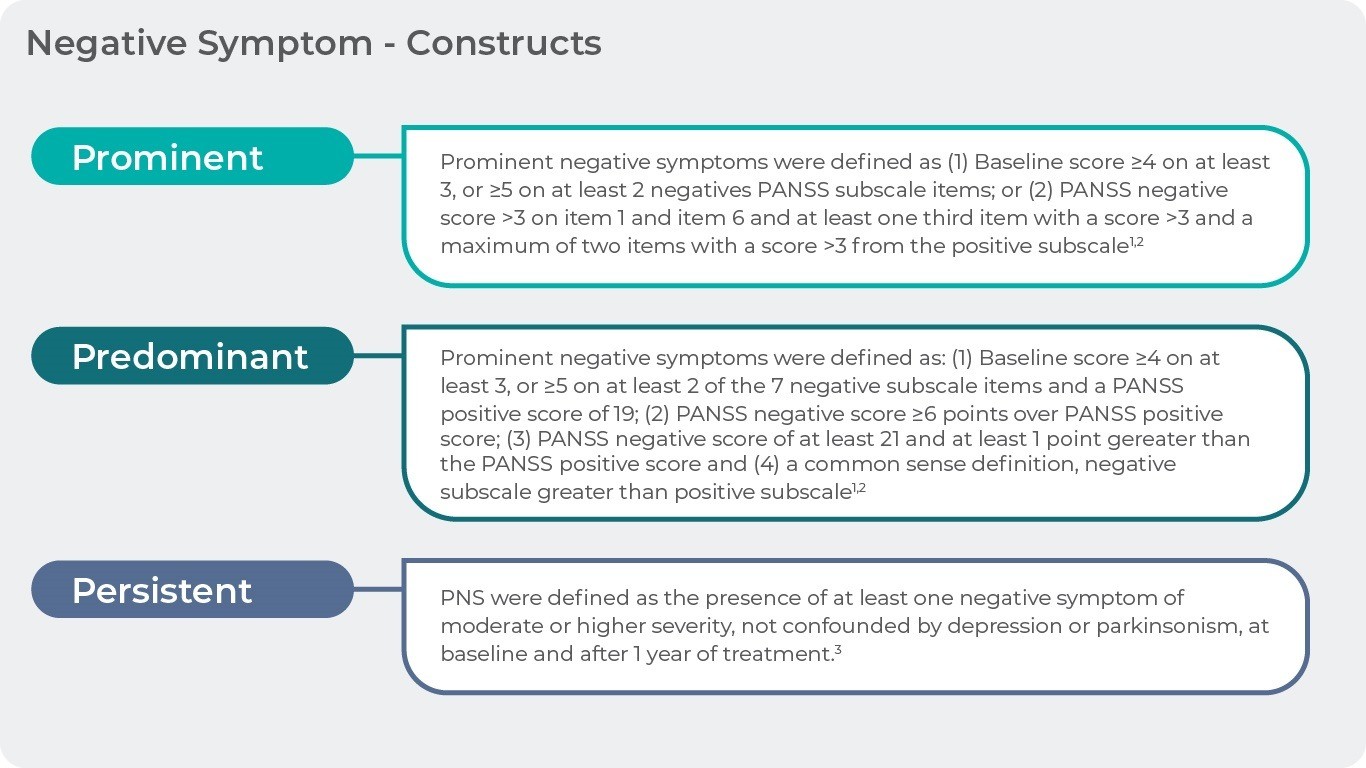
Negative symptoms can further be characterized based on their cause (primary, secondary), intensity (prominent, predominant) or duration (persistent).
| Negative symptom dimensions | |
| Primary | Cause factor: schizophrenia, core symptom |
| Secondary | Cause factor: other symptoms of schizophrenia, depression, environment |
| Prominent | Intensity factor: more negative symptoms than positive symptoms |
| Predominant | Intensity factor: high level of negative symptoms, low positive symptoms |
| Persistent | Time factor: present for more than 6 months – 1 year |
Primary negative symptoms are considered core symptoms of schizophrenia which persist during clinical stability and have an own pathophysiology15. In contrast secondary negative symptoms are a consequence of other symptoms such as positive symptoms, neurological side effects, depressive symptoms, or environmental factors16,17.
The qualities of “prominent” and “predominant” describe the intensity of the negative symptoms in a given patient. Symptoms are “prominent” if there are more negative than positive symptoms present in the patients (Criteria: 1. Baseline score ≥4 on at least 3, or ≥5 on at least 2 negative PANSS subscale items; or 2. PANSS negative score >3 on item 1 and item 6 and at least one third item with a score >3 and a maximum of two items with a score >3 from the positive subscale)18,19.
Symptoms are “predominant” if they dominate the clinical picture while positive symptoms are only marginally present (Criteria: 1. Baseline score ≥4 on at least 3 or ≥5 on at least 2 of the 7 negative subscale items and a PANSS positive score of <19; 2. PANSS negative score ≥6 points over PANSS positive score; 3. PANSS negative score of at least 21 and at least 1 point greater than the PANSS positive score and 4. A common sense definition, negative subscale greater than positive subscale)18,19.
Persistent negative symptoms are defined as at least one negative symptom of moderate or higher severity that is present for more than one year20. For the purposes of clinical studies more than 6 months is required19.
References
- Kirkpatrick, B., Fenton, W. S., Carpenter, W. T. & Marder, S. R. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr. Bull. 32, 214–219 (2006).
- Wallwork, R. S., Fortgang, R., Hashimoto, R., Weinberger, D. R. & Dickinson, D. Searching for a consensus five-factor model of the Positive and Negative Syndrome Scale for schizophrenia. Schizophr. Res. 137, 246–250 (2012).
- Foussias, G., Agid, O., Fervaha, G. & Remington, G. Negative symptoms of schizophrenia: Clinical features, relevance to real world functioning and specificity versus other CNS disorders. Eur. Neuropsychopharmacol. 24, 693–709 (2014).
- Bleuler, E. Dementia praecox or the group of schizophrenias. Dementia praecox or the group of schizophrenias (1950).
- National Institutes of Mental Health (NIMH). Schizophrenia. (2017). Available at: https://www.nimh.nih.gov/health/publications/schizophrenia-booklet/index.shtml.
- Fischer, B. A. & Buchanan, R. W. Schizophrenia: Clinical Manifestations, Course, Assessment and Diagnosis. UpToDate (2017). Available at: www.up-to-date/schizophrenia.
- Marder, S. R. & Galderisi, S. The current conceptualization of negative symptoms in schizophrenia. World Psychiatry 16, 14–24 (2017).
- Strauss, G. P., Waltz, J. A. & Gold, J. M. A review of reward processing and motivational impairment in schizophrenia. Schizophr. Bull. 40, S107-116 (2014).
- Lyne, J. et al. Prevalence of item level negative symptoms in first episode psychosis diagnoses. Schizophr. Res. 135, 128–133 (2012).
- Peralta, V. & Cuesta, M. J. Dimensional structure of psychotic symptoms: An item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr. Res. 38, 13–26 (1999).
- Selten, J. P., Wiersma, D. & Van den Bosch, R. J. Distress attributed to negative symptoms in schizophrenia. Schizophr. Bull. 26, 737–744 (2000).
- Fleischhacker, W. et al. The efficacy of cariprazine in negative symptoms of schizophrenia: Post hoc analyses of PANSS individual items and PANSS-derived factors. Eur. Psychiatry 58, 1–9 (2019).
- Bucci, P. & Galderisi, S. Categorizing and assessing negative symptoms. Curr. Opin. Psychiatry 30, 201–208 (2017).
- Liemburg, E. et al. Two subdomains of negative symptoms in psychotic disorders: Established and confirmed in two large cohorts. J. Psychiatr. Res. 47, 718–725 (2013).
- Mucci, A., Merlotti, E., Üçok, A., Aleman, A. & Galderisi, S. Primary and persistent negative symptoms: Concepts, assessments and neurobiological bases. Schizophr. Res. 186, 19–28 (2017).
- Carpenter, W. T., Heinrichs, D. W. & Alphs, L. D. Treatment of negative symptoms. Schizophr. Bull. 11, 440–452 (1985).
- Hasan, A. et al. World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for Biological Treatment of Schizophrenia, Part 1: Update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J. Biol. Psychiatry 13, 318–378 (2012).
- Rabinowitz, J. et al. Negative symptoms in schizophrenia – the remarkable impact of inclusion definitions in clinical trials and their consequences. Schizophr. Res. 150, 334–338 (2013).
- European Medicines Agency. Guideline on clinical investigation of medicinal products, including depot preparation in the treatment of schizophrenia. (2012).
- Galderisi, S. et al. Persistent negative symptoms in first episode patients with schizophrenia: Results from the European First Episode Schizophrenia Trial. Eur. Neuropsychopharmacol. 23, 196–204 (2013).
Acta Psychiatrica Scandinavica
Negative symptoms of schizophrenia: a problem that won’t go away.

Negative Symptoms: What are these?
Negative symptoms can be clustered in 2 or 5-factor models: diminished emotional expression (affect blunted, alogia) and reduced motivation and pleasure (anhedonia, asociality, avolition). Download the easy visual here
DownloadReferences title
Negative Symptoms: Primary vs. Secondary

Negative Symptoms – Constructs
NEGATIVE SYMPTOMS – THE CHALLENGENEGATIVE SYMPTOMS – THE CHALLENGE
Although negative symptoms have long been recognized as an independent symptom domain, distinct from positive symptoms, neurocognition, and social cognition, thAlthough negative symptoms have long been recognized as an independent symptom domain, distinct from positive symptoms, neurocognition, and social cognition, th
more…REAGILA AND DAILY FUNCTIONINGOUR PRODUCT AND DAILY FUNCTIONING
Negative symptom improvement must be accompanied by improved patient functioning in order for change to be considered clinically relevant in patients with schizNegative symptom improvement must be accompanied by improved patient functioning in order for change to be considered clinically relevant in patients with schiz
more…
