REAGILA in The Long-Term Treatment of Schizophrenia
- Cariprazine is an effective long-term treatment1
- Cariprazine prevents relapse and sustains remission over long-term treatment in patients with schizophrenia1,2
- Given its long-half life, a patient may be able to miss occasional doses of cariprazine and maintain efficacy nonetheless3
In this section
After Symptoms Are Controlled Acutely…
Atypical antipsychotics need to be effective across the span of illness in patients with schizophrenia10. When patients experience acute exacerbation of psychotic symptoms during relapse, they risk detrimental effects that could affect their brain integrity and impair long-term outcomes4-6. Continuous prophylactic antipsychotic treatment reduces the risk of relapse by approximately 70% in patients with schizophrenia7, illustrating why medication noncompliance is considered the most important factor related to relapse8. Lapses in medication as short as 1 to 10 days are associated with an increased risk of hospitalization9, which suggests that exacerbation and relapse may occur quickly without antipsychotic activity.
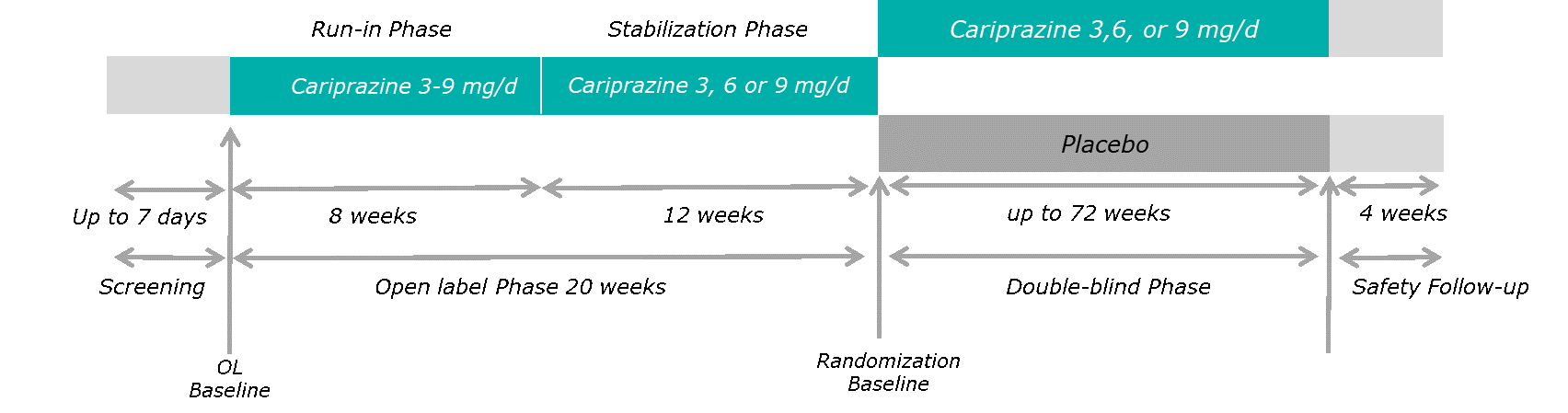
Long-Term Efficacy With Cariprazine (ClinicalTrials.gov Identifier: NCT01412060; EUDRA CT Number: 2011-002048-29)1
Long-term treatment with cariprazine has been evaluated in one clinical study of relapse prevention in patients with schizophrenia10. In this phase 3, multinational, multicentre, randomized, double-blind, placebo-controlled, parallel-group, flexible- and fixed-dose study, patients with acute symptoms of schizophrenia were stabilized on 20 weeks of open-label cariprazine 3-9 mg/d treatment (although the finally approved dose-range is 1.5-6 mg/day)10. Eligible patients were randomized (1:1) to double-blind placebo (n=99) or cariprazine (n=101) where they received the same dose of cariprazine as during the stabilization phase10. Double-blind treatment lasted up to 72 weeks and ended for all active patients when the last randomized patient completed 26 weeks of treatment, or at early termination (including relapse)1.
Reference: Durgam, S. et al. Long-term cariprazine treatment for the prevention of relapse in patients with schizophrenia: A randomized, double-blind, placebo-controlled trial. Schizophr. Res. 176, 264–271 (2016)1 (Graphic elaboration from text data)
The primary efficacy endpoint was time to first relapse during double-blind treatment. Relapse was defined as meeting any one of the following clinical or rating scale criteria1:
| Rating scale criteria | Clinical relapse criteria |
| Increase ≥30% in PANSS total score for patients who scored ≥50 at randomization or a ≥10 point increase for patients who scored <50 at randomization | Psychiatric hospitalization due to worsening of schizophrenia |
| Score >4 on any PANSS item assessed at randomization: delusions, conceptual disorganization, hallucinatory behavior, suspiciousness/persecution, hostility, uncooperativeness, poor impulse control | Deliberate self-injury or aggressive/violent behavior |
| CGI-S score increase ≥2 points from randomization | Clinically significant suicidal/homicidal ideation |
CGI-S = Clinical Global Impressions-Improvement; PANSS= Positive and Negative Syndrome Scale.
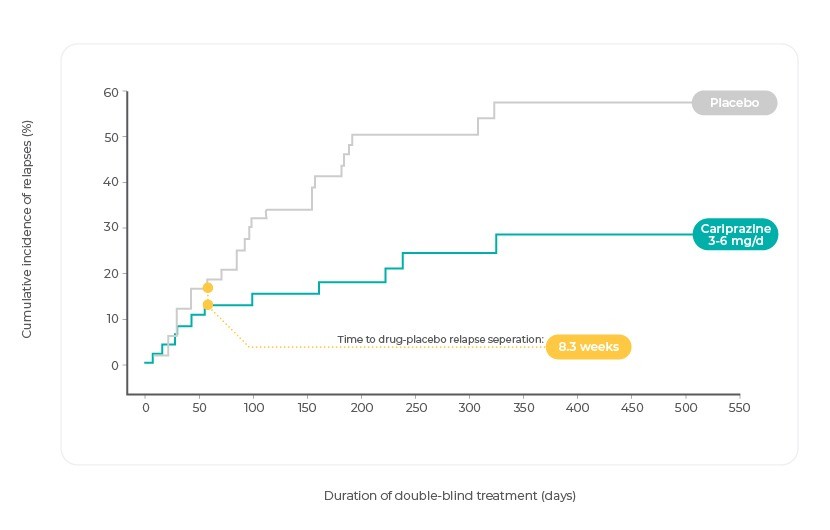
Time to Relapse Was Significantly Longer With Cariprazine Versus Placebo
During double-blind treatment, the time to relapse was significantly longer with cariprazine than with placebo (HR = 0.45 [95% confidence interval, 0.28–0.73], P=.001)10. Only 24.8% of cariprazine-treated patients compared with 47.5% of placebo-treated patients met relapse criteria, yielding a number needed to treat of 51,10. Treatment with cariprazine doses within this range (ie, 3–6 mg/d) was also associated with a significantly delayed time to relapse compared with the corresponding placebo group (ie, participants that were stabilized on cariprazine 3–6 mg/d during the open-label phase; P=0.026, HR [95% CI]=0.49 [0.25, 0.93])3,10.
Kaplan-Meier Curve of Cumulative Rate of Relapse During the Double-Blind Treatment Period
References: Adapted from Correll, C. U., Jain, R. & Meyers, J. E. Relationship between the timing of relapse and plasma drug levels following discontinuation of cariprazine treatment in patients with schizophrenia: indirect comparison with other second-generation antipsychotics after treatment discontinuation. Neuropsychiatr. Dis Treat 15, 2537–2550 (2019)3.
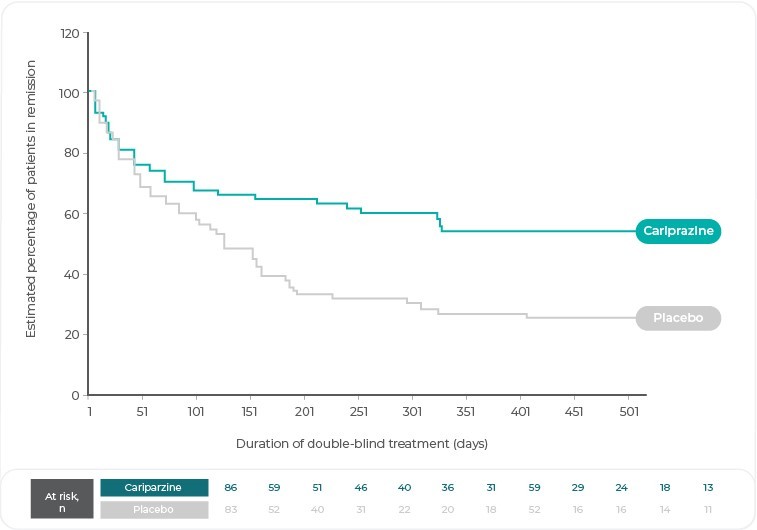
Sustained Remission Was Significantly Longer With Cariprazine Versus Placebo
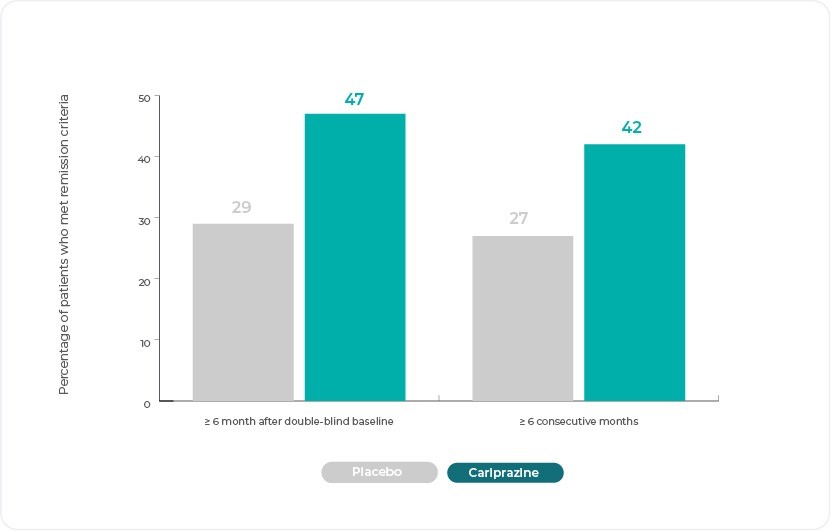
Long term remission, just as prevention of relapse, is a long-term treatment goal in schizophrenia. Sustained remission is a critical concept of treatment response that emphasizes symptom stability over prolonged periods of time for patients with schizophrenia. The Remission in Schizophrenia Working Group (RSWG) developed operational criteria for remission that consist of a symptomatic component and a time component. The symptomatic component requires that patients have scores corresponding to a severity level of mild or better (≤ 3) on 8 individual items of the PANSS; while the time component requires that symptomatic criteria be met for ≥ 6 consecutive months. Importantly, this definition of remission uses an absolute threshold of symptom severity, not a degree of improvement from a baseline score2.
Symptomatic remission for the analyses was defined as a score ≤ 3 (mild) on the following 8 PANSS items: mannerisms and posturing (G5), unusual thought content (G9), blunted affect (N1), social withdrawal (N4), lack of spontaneity (N6), delusions (P1), conceptual disorganization (P2), and hallucinatory behaviour (P3). Sustained remission included meeting remission criteria at the current and all prior double-blind visits or for ≥ 6 consecutive months. Loss of remission was defined as patients who no longer met remission criteria or who discontinued due to relapse2.
During double-blind treatment, time to loss of sustained remission was significantly longer (P = .0020) for cariprazine versus placebo (hazard ratio = 0.51); 60.5% of cariprazine-treated and 34.9% of placebo-treated patients sustained remission through the final visit (odds ratio [OR] = 2.85; P = .0012; number needed to treat [NNT] = 4)10. Almost twice as many cariprazine-treated (39.6%) as placebo-treated (21.2%) patients met symptomatic remission criteria at all visits ≥ 6 consecutive months immediately before/including the final double-blind visit (OR = 2.44; P = .0057; NNT = 6)10. More cariprazine-treated (41.6%) than placebo-treated (27.3%) patients sustained remission for any ≥ 6 consecutive month period (OR = 1.90, P = .0379; NNT = 7)2,10.
Reference: Adapted from Correll, C. U. et al. Long-term remission with cariprazine treatment in patients with schizophrenia: A post hoc analysis of a randomized, double-blind, placebo-controlled, relapse prevention trial. J. Clin. Psychiatry 80, 18m12495 (2019)2.
Reference: Adapted from Correll, C. U. et al. Long-term remission with cariprazine treatment in patients with schizophrenia: A post hoc analysis of a randomized, double-blind, placebo-controlled, relapse prevention trial. J. Clin. Psychiatry 80, 18m12495 (2019)2.
What About the Long Half-Life?
Cariprazine and its active metabolites have a half-life of 1 to 3 weeks, which is considerably longer than any other oral antipsychotic agent (7-91 hours)3,10. For patients switched to placebo after open-label cariprazine treatment, only 5% of patients relapsed during the first 4 weeks of double-blind treatment in the cariprazine relapse prevention study compared with 8%–34% of patients in relapse prevention studies of other atypical antipsychotics10. Additionally, the drug and placebo Kaplan-Meier curves separated at 6-7 weeks after randomization for cariprazine, while separation of the curves for other atypical antipsychotics occurred earlier (1-4 weeks)10. This was also true for the recommended 3–6 mg/d dose range: the time to separation of the drug-placebo curves occurred even later (8.3 weeks) in these patients3.
Collectively, these results suggest that residual treatment effects are present after cariprazine discontinuation10. This has clinical relevance, since cariprazine will remain at a therapeutic level and continue exerting its effect, even if patients intermittently miss a few doses of their medication3,10.
References
- Durgam, S. et al. Long-term cariprazine treatment for the prevention of relapse in patients with schizophrenia: A randomized, double-blind, placebo-controlled trial. Schizophr. Res. 176, 264–271 (2016).
- Correll, C. U. et al. Long-term remission with cariprazine treatment in patients with schizophrenia: A post hoc analysis of a randomized, double-blind, placebo-controlled, relapse prevention trial. J. Clin. Psychiatry 80, 18m12495 (2019).
- Correll, C. U. et al. Relationship between the timing of relapse and plasma drug levels following discontinuation of cariprazine treatment in patients with schizophrenia: Indirect comparison with other second-generation antipsychotics after treatment discontinuation. Neuropsychiatr. Dis. Treat. 15, 2537–2550 (2019).
- Shepherd, M., Watt, D., Falloon, I. & Smeeton, N. The natural history of schizophrenia: a five-year follow-up study of outcome and prediction in a representative sample of schizophrenics. Psychol. Med. Monogr. Suppl. Monograph, 1–46 (1989).
- Cahn, W. et al. Psychosis and brain volume changes during the first five years of schizophrenia. Eur. Neuropsychopharmacol. 19, 147–151 (2009).
- Andreasen, N. C., Liu, D., Ziebell, S., Vora, A. & Ho, B. C. Relapse duration, treatment intensity, and brain tissue loss in schizophrenia: A prospective longitudinal MRI study. Am. J. Psychiatry 170, 609-615- (2013).
- Lindenmayer, J. P. et al. Medication nonadherence and treatment outcome in patients with schizophrenia or schizoaffective disorder with suboptimal prior response. J. Clin. Psychiatry 70, 990–996 (2009).
- Ayuso-Gutiérrez, J. L. & Del Río Vega, J. M. Factors influencing relapse in the long-term course of schizophrenia. Schizophr. Res. 28, 199–206 (1997).
- Weiden, P. J., Kozma, C., Grogg, A. & Locklear, J. Partial compliance and risk of rehospitalization among California medicaid patients with schizophrenia. Psychiatr. Serv. 55, 886–891 (2004).
- Reagila SmPC.
CNS Spectrums
Mechanism of action of cariprazine
HOW DOES REAGILA WORK?HOW DOES OUR PRODUCT WORK?
Cariprazine has high affinity for dopamine D3 and D2 receptors as well as serotonin 5 HT2B and 5 HT1A receptors, moderate affinity to 5 HT2A, histamine H1, and Find out more about its mechanism of action
more…REAGILA IN ACUTE SCHIZOPHRENIAOUR PRODUCT IN ACUTE SCHIZOPHRENIA
Once the diagnosis of schizophrenia is made, clinicians, patients, and families have important treatment decisions to make. Although it seems intuitive to say tOnce the diagnosis of schizophrenia is made, clinicians, patients, and families have important treatment decisions to make. Although it seems intuitive to say t
more…