Mechanism of Action of Antipsychotics – How Do They Work?
- The key role in antipsychotic efficacy is dopamine D2 receptor blockade, which all antipsychotics exhibit to differing degrees.
- First- (typical) and second-generation (atypical) antipsychotics are antagonists at dopamine D2 receptors.
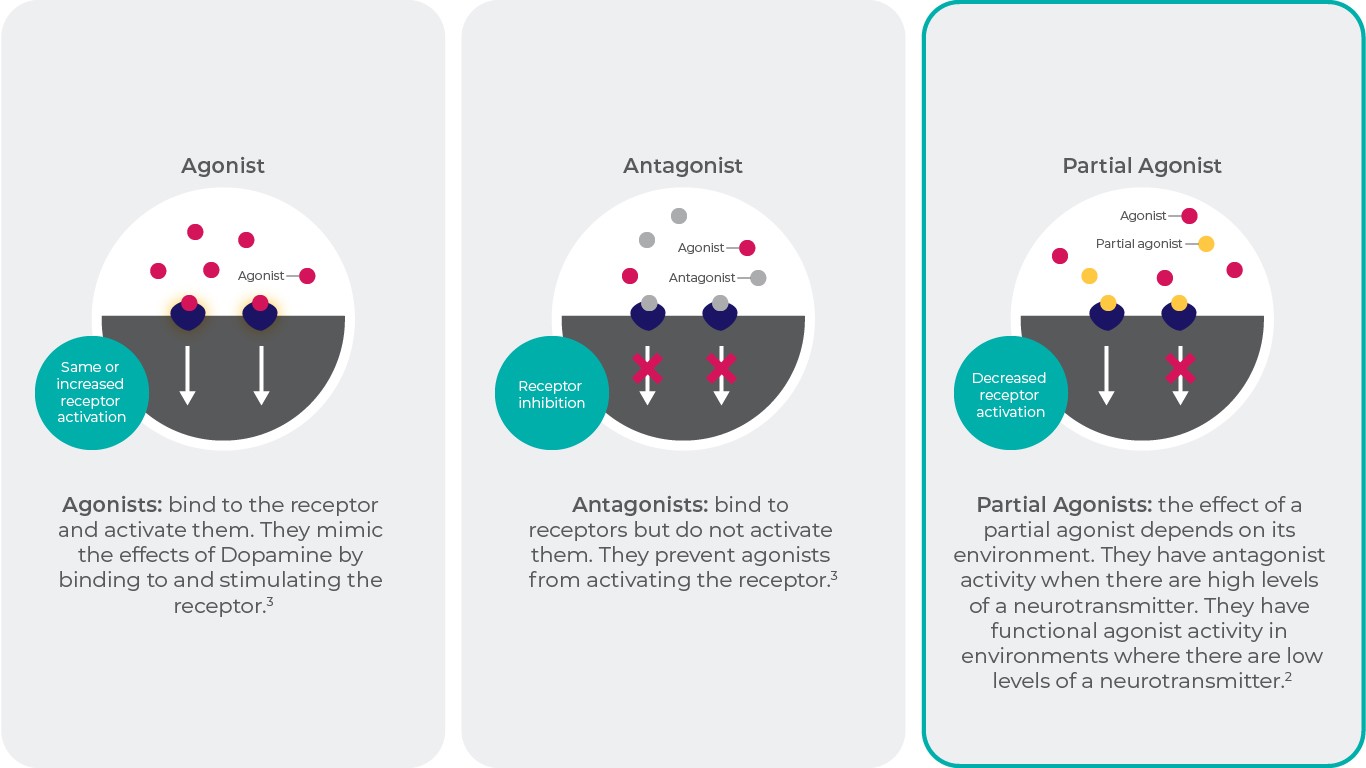
- Compounds that act as dopamine receptor partial agonists represent a third generation of antipsychotics.
- Dopamine receptor partial agonist activity differs depending on the level of the naturally occurring dopamine in the brain.
- Partial agonists display functional antagonist activity at target receptors when neurotransmitter levels are high, and display functional agonist activity when neurotransmitter levels are low.
In this section
Antipsychotics are the cornerstone of treatment for schizophrenia. Since the 1950s, when chlorpromazine was serendipitously discovered, the design and development of these drugs have led to more than 30 different antipsychotics being approved. Although the receptor affinity profiles of these drugs differ considerably, all antipsychotics show considerable binding to dopamine D2 receptors at therapeutic doses—this binding mechanism is essential for therapeutic efficacy1.
Antipsychotic Classes
The clinical efficacy profile of typical antipsychotic agents appears to depend on high affinity for and full antagonist activity at dopamine D2 receptors. Due to this receptor binding profile, typical antipsychotics are effective for the treatment of positive symptoms of schizophrenia, but they are unable to alleviate negative symptoms and cognitive impairments, which are also associated with schizophrenia. Therapeutic doses of these drugs also cause high rates of extrapyramidal symptoms (EPS), an adverse effect caused by antagonizing dopamine receptors in the nigrostriatal pathway2.
Like typical antipsychotics, atypical antipsychotics are antagonists at D2 receptors, though they are characterized by a lower liability for EPS and bind to a diverse range of neuroreceptor types2. For example, several of these drugs have high serotonin 5-HT2A receptor affinity relative to dopamine D2 and D3 receptor blockade1.
Typical and atypical antipsychotics both act as full antagonists at D2 receptors, although they have markedly different affinities. The wide range of symptoms associated with schizophrenia are thought to result from a combination of overactive and underactive dopaminergic pathways. Additionally, antagonist activity at dopaminergic pathways that are not as heavily involved in schizophrenia pathophysiology, such as the nigrostriatal or tuberoinfundibular pathways, can lead to severe adverse effects, such as EPS and hyperprolactinemia, and the worsening of negative and cognitive symptoms. Given these complications, a drug that can alter dopamine neurotransmission differently under various physiological conditions may offer therapeutic and safety advantages over currently available antipsychotics2. A partial agonist may capable of doing so—antipsychotics, such as aripiprazole, brexpiprazole, and cariprazine, that act via partial agonism at dopamine D2 and D3 receptors represent a third generation of antipsychotics1,14.
So, What’s a Partial Agonist?
Partial agonists can act as either a functional agonist or a functional antagonist depending on the levels of the full agonist (eg, the endogenous neurotransmitter) present in the surrounding environment. Compared with full agonists, partial agonists have lower intrinsic activity. In the absence of a full agonist, partial agonists can bind to the receptor to produce a response, showing functional agonist activity; however, in the presence of a full agonist, the receptor binding of a partial agonist reduces the agonist’s response, showing functional antagonist activity2,3.
References: Adapted from Lieberman, J. A. Dopamine partial agonists: A new class of antipsychotic. CNS Drugs 18, 251–267 (2004)2; Lambert, D. G. Drugs and receptors. Contin. Educ. Anaesthesia, Crit. Care Pain 4, 181–184 (2004)3.
Thus, partial agonism at dopamine D2 receptors offers an appealing option for treating the symptoms of schizophrenia. A partial agonist should act as a functional antagonist in the mesolimbic pathway, where excessive dopamine activity is believed to cause positive symptoms, but a partial agonist should act as a functional agonist in the mesocortical pathway, where reduced dopamine activity may be associated with negative symptoms and cognitive impairment. In addition, partial agonism may also avoid complete blockade of the dopamine pathways associated with EPS and elevated prolactin levels2.
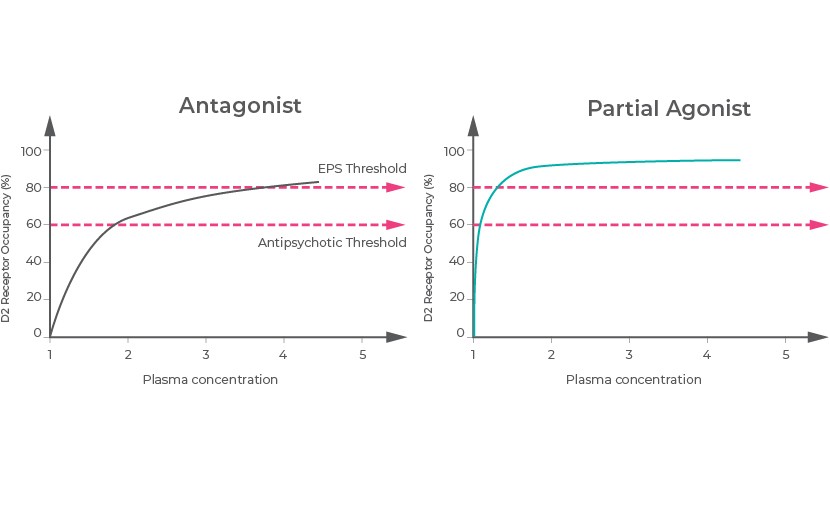
The Basic Antipsychotic Action
For a clinical response, a minimum of 50% occupancy of dopamine D2 receptors by antipsychotics is generally required, while occupancy above 85% results in an increased the risk of EPS and other undesirable side effects. This suggests that there is a therapeutic window between 60% and 80% for dopamine D2 receptor occupancy that balances a high likelihood of clinical response with low risk of EPS. Only clozapine and partial agonists at dopamine receptors have been shown to be exceptions to this generalization1.
Clozapine results in lower striatal dopamine D2 receptor occupancy (~40%) at clinical, which infers something about its mechanism of action and safety profile. In contrast, aripiprazole and cariprazine occupy a higher proportion (80% or more) of D2 receptors at therapeutic doses14. Consequently, antipsychotics that are partial agonists require higher dopamine D2 receptor occupancy levels to have a clinical effect than what is needed for dopamine antagonists. This may be due to these partial agonists having lower intrinsic activity compared with dopamine at D2 receptors, resulting in net functional antagonism, which ends up being similar to the behavior of antagonists at therapeutic doses1.
Reference: Adapted from Kaar, S. J., Natesan, S., McCutcheon, R. & Howes, O. D. Antipsychotics: Mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacology (2019)1
However, it is difficult to describe intrinsic activity numerically since there is great variability between assay conditions. There is also the fact that in vitro measurements cannot capture in vivo conditions as these receptors are not isolated but instead interact with multiple other receptors and transduction proteins6.
Efficacy at Different Dopamine Receptors
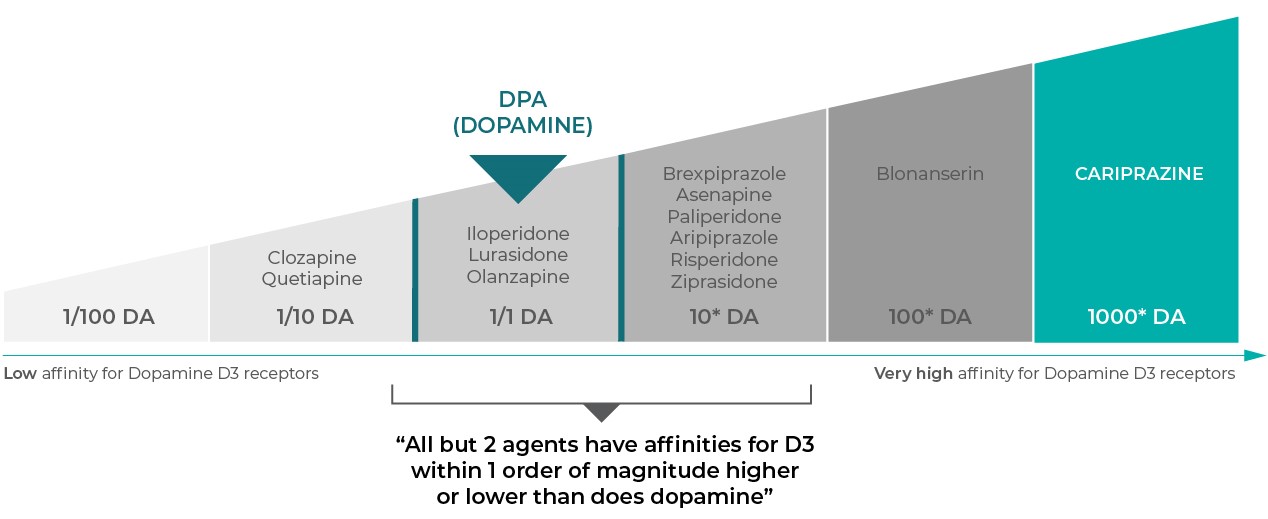
All antipsychotics can bind to dopamine D2 receptors; however, some of these agents also show affinity for dopamine D1 and D3 receptors. In general, clinically relevant binding at dopamine receptors is dependent on its relative potency compared with the endogenous dopamine at these receptors (for example, if an antipsychotic drug has a lower binding affinity than dopamine, it is unlikely to elicit an effect). With regards to activity at D1 and D3 receptors, clinical relevance is also dependent on the relative potency of the binding at these receptors compared with the binding potency at the D2 receptors. For example, if a drug has a lower affinity for D1 and/or D3 compared with D2 receptors, then the effect at D2 receptors will likely dominate over that at the D1 and/or D3 receptors11.
Many antipsychotics have D3 receptor affinity that is about the same as or higher than affinity for the D2 receptor and generally lower than the D3 receptor affinity of dopamine itself. The latter point suggests that only minimal or no D3 receptor occupancy would be expected in dopamine-rich brain areas by drugs other than those with the most potent binding to D3. In other words, drugs need to have D3 receptor affinity that is even higher than that of dopamine itself to be clinically relevant. As such, the only agents that are likely to have clinically meaningful degrees of D3 receptor occupancy when dosed for psychosis are the D3-preferring agent cariprazine and perhaps blonanserin (a drug for psychosis marketed in Japan)12,14. Reduced limbic dopamine release has been hypothesized to be linked to anhedonia, depressive states, motivation, and pleasure. Results from animal models are consistent with this idea, showing that D3 antagonism improves cognition, mood, and motivation; clinical results also suggest enhanced efficacy in negative symptoms of schizophrenia for cariprazine12,14.
D3 Receptor Affinity11,12
Reference: Adapted from Stahl, S. M. Drugs for psychosis and mood: Unique actions at D3, D2, and D1 dopamine receptor subtypes. CNS Spectr. 22, 375–384 (2017)12
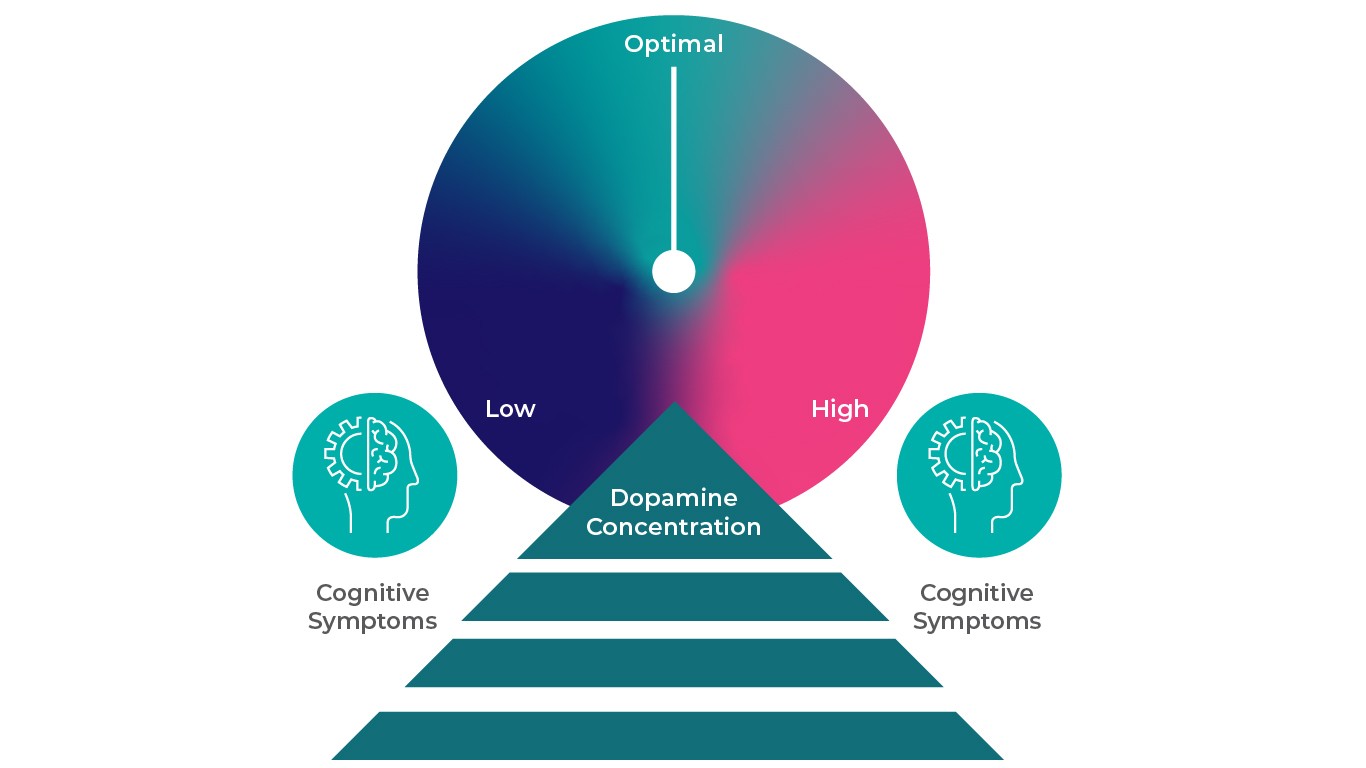
Beyond the D2 and D3 receptors1, other dopamine receptors may also have significant effects. For example, dopamine D1 receptors are thought to play a role in attention, working memory, and executive function. Theoretically, drugs that block or overstimulate D1 receptors could dysregulate D1 receptors, which could hypothetically lead to cognitive dysfunction. Cognitive dysfunction would clearly be an undesired effect of agents that block D1 receptors, especially in patients with disorders characterized by cognitive dysfunction, such as schizophrenia and bipolar disorder. Dopamine D1 receptor occupancy varies widely among antipsychotics at clinically effective doses; for example, occupancy levels are 0% with haloperidol, ~25% with risperidone, and up to ~60% with clozapine1. Some drugs have dopamine D1 receptor affinities that are close to their D2 receptor affinities and greater than dopamine’s affinity for D1 receptors (which is relatively low), suggesting potentially clinically relevant occupancy at D1 receptors at therapeutic doses12. Some of the drugs that potentially exhibit clinically relevant blockade of D1 receptors also block muscarinic cholinergic and histamine receptors to varying degrees, which in theory adds to the potential for treating cognitive dysfunction. Whether D1 antagonism has any potential benefit remains to be shown12.
When Dopamine Concentrations in the PFC are Too High or Too Low, Cognitive Deficits May Arise13
References: Adapted from Cools, R. & D’Esposito, M. Inverted-U-shaped dopamine actions on human working memory and cognitive control. Biol. Psychiatry 69, e113-125 (2011)13.
D4 receptors are found in similar brain regions as D2 receptors but likely at lower concentrations. Clozapine is unique because due to its high affinity for D4 receptors relative to its affinity for dopamine D2 receptors; as such, it should have a higher proportion of dopamine D4 receptors occupied at clinically effective doses compared with other antipsychotics. In practice, however, selective dopamine D4 receptor antagonists have not shown efficacy as antipsychotics to date1.
Additionally, the effects of D5 receptors are not well understood.
References
- Kaar, S. J., Natesan, S., McCutcheon, R. & Howes, O. D. Antipsychotics: Mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology. Neuropharmacology (2019). doi:10.1016/j.neuropharm.2019.107704
- Lieberman, J. A. Dopamine partial agonists: A new class of antipsychotic. CNS Drugs 18, 251–267 (2004).
- Lambert, D. G. Drugs and receptors. Contin. Educ. Anaesthesia, Crit. Care Pain 4, 181–184 (2004).
- Tadori, Y., Forbes, R. A., McQuade, R. D. & Kikuchi, T. Receptor reserve-dependent properties of antipsychotics at human dopamine D2 receptors. Eur. J. Pharmacol. 607, 35–40 (2009).
- Tadori, Y. et al. Differences in agonist/antagonist properties at human dopamine D 2 receptors between aripiprazole, bifeprunox and SDZ 208-912. Eur. J. Pharmacol. 574, 103–111 (2007).
- Tadori, Y. et al. Aripiprazole’s low intrinsic activities at human dopamine D2L and D2S receptors render it a unique antipsychotic. Eur. J. Pharmacol. 515, 10–19 (2005).
- Tadori, Y., Forbes, R. A., McQuade, R. D. & Kikuchi, T. Functional potencies of dopamine agonists and antagonists at human dopamine D 2 and D 3 receptors. Eur. J. Pharmacol. 666, 43–52 (2011).
- Tadori, Y., Forbes, R. A., McQuade, R. D. & Kikuchi, T. In vitro pharmacology of aripiprazole, its metabolite and experimental dopamine partial agonists at human dopamine D 2 and D 3 receptors. Eur. J. Pharmacol. 355–365 (2011). doi:10.1016/j.ejphar.2011.07.020
- Koener, B., Focant, M. C., Bosier, B., Maloteaux, J. M. & Hermans, E. Increasing the density of the D 2L receptor and manipulating the receptor environment are required to evidence the partial agonist properties of aripiprazole. Prog. Neuro-Psychopharmacology Biol. Psychiatry 36, 60–70 (2012).
- Urban, J. D., Vargas, G. A., Von Zastrow, M. & Mailman, R. B. Aripiprazole has functionally selective actions at dopamine D2 receptor-mediated signaling pathways. Neuropsychopharmacology 32, 67–77 (2007).
- Stahl, S. M. Dazzled by the dominions of dopamine: Clinical roles of D3, D2, and D1 receptors. CNS Spectr. 22, 305–311 (2017).
- Stahl, S. M. Drugs for psychosis and mood: Unique actions at D3, D2, and D1 dopamine receptor subtypes. CNS Spectr. 22, 375–384 (2017).
- Cools, R. & D’Esposito, M. Inverted-U-shaped dopamine actions on human working memory and cognitive control. Biol. Psychiatry 69, e113-125 (2011).
- Reagila SmPC.
Neuropharmacology
Antipsychotics: Mechanisms underlying clinical response and side-effects and novel treatment approaches based on pathophysiology.
HOW DOES REAGILA WORK?HOW DOES OUR PRODUCT WORK?
Cariprazine has high affinity for dopamine D3 and D2 receptors as well as serotonin 5 HT2B and 5 HT1A receptors, moderate affinity to 5 HT2A, histamine H1, and Find out more about its mechanism of action
more…SCHIZOPHRENIA: NEUROCHEMICAL BASISSCHIZOPHRENIA: NEUROCHEMICAL BASIS
The dopamine hypothesis of schizophrenia began as a theory based on circumstantial evidence obtained from clinical observations following antipsychotic treatmenThe dopamine hypothesis of schizophrenia began as a theory based on circumstantial evidence obtained from clinical observations following antipsychotic treatmen
more…