Clinical guide for treating negative symptoms in schizophrenia
- Negative symptoms in schizophrenia cause patients to have poor functional outcomes and long-term disability, as they are a core component of the illness
- Limited treatment options are available for negative symptoms
- To date, Cariprazine is the only antipsychotic that has demonstrated superiority over another antipsychotic for the treatment of negative symptoms in schizophrenia in a prospective, large-scale, randomized, double-blind clinical study.
- Psychosocial treatments, although showing mixed and inconsistent results, may improve outcomes and quality of life and help patients cope with negative symptoms
In this section
This article by Correll et al. aims to provide useful information for physicians about treating negative symptoms in schizophrenia. A multistep PubMed and Google Scholar literature search on the phrase “negative symptoms schizophrenia” was used to find review articles and metanalyses published from 2009–2019. Also, to find articles outside of the computerized search, a manual search of reference lists of relevant reviews and primary studies were conducted. The article summarizes the definitions and terms that surround negative symptoms and expresses that schizophrenia patients have poor functional outcomes and long-term disability because negative symptoms are a central component of the illness.
The article explains that “to date, no agent is approved by the FDA for the treatment of negative symptoms” and points out that “to date, the only prospective, large-scale, randomized, double-blind evidence demonstrating the superiority of one approved antipsychotic over another in the treatment of negative symptoms comes from a rigorously designed 26- week study comparing the effects of fixed-dose cariprazine (3 mg/d, 4.5 mg/d [target dose], or 6 mg/d) and risperidone (3 mg/d, 4 mg/d [target dose], or 6 mg/d) on predominant negative symptoms in patients with stable and limited positive symptoms, and without relevant depression or extrapyramidal symptoms.” The study showed that cariprazine, a dopamine D3-preferring D3/D2 receptor partial agonist and serotonin 5-HT1A receptor partial agonist, has significant differences and clinically relevant improvement in both negative symptoms and functional impairment compared to risperidone. Cariprazine also showed significant advantages over risperidone on the Clinical Global Impressions-Improvement Scale (CGI-I) and the Personal and Social Performance Scale (PSP), further demonstrating that it can be a clinically meaningful treatment for negative symptoms.
Other adjunctive treatments against negative symptoms, such as glutamatergic compounds (e.g., glycine, D-serine, D-cycloserine), minocycline, dopamine agonists (e.g., selegiline, modafinil), and cholinergics, have shown limited evidence thus far. The article calls for higher-quality trials and patient-based meta-analyses to examine whether patients might benefit from combination treatment, as there is currently no single co-treatment strategy with sufficient evidence to treat negative symptoms. Agents acting on NMDA receptors, alpha 7 nicotinic receptors, and 5-HT2A and sigma-2 receptors, antidepressants, deep transcranial magnetic stimulation and transcranial direct current stimulation are all under investigation for negative symptoms treatment.
Some strategies that have shown some benefits in improving negative symptoms:
Cognitive behavioural therapy (CBT), as an adjunct to antipsychotic treatment has “demonstrated positive, but moderate, effects on negative symptoms, with a reduction of apathy and improved motivation.”
The article suggests that “a focus on healthy lifestyles, with emphasis on exercise, sleep, diet, smoking cessation, appropriate alcohol consumption, and social participation, should always be suggested in the course of treatment.”
Family interventions have also shown some benefit
Motivation and Enhancement Training (MOVE), “a novel treatment that combines environmental support, CBT, skills training, and other psychosocial modalities, has also been assessed as a specific negative symptom intervention, with preliminary results suggesting some improvement, but only after 9 months of therapy.”
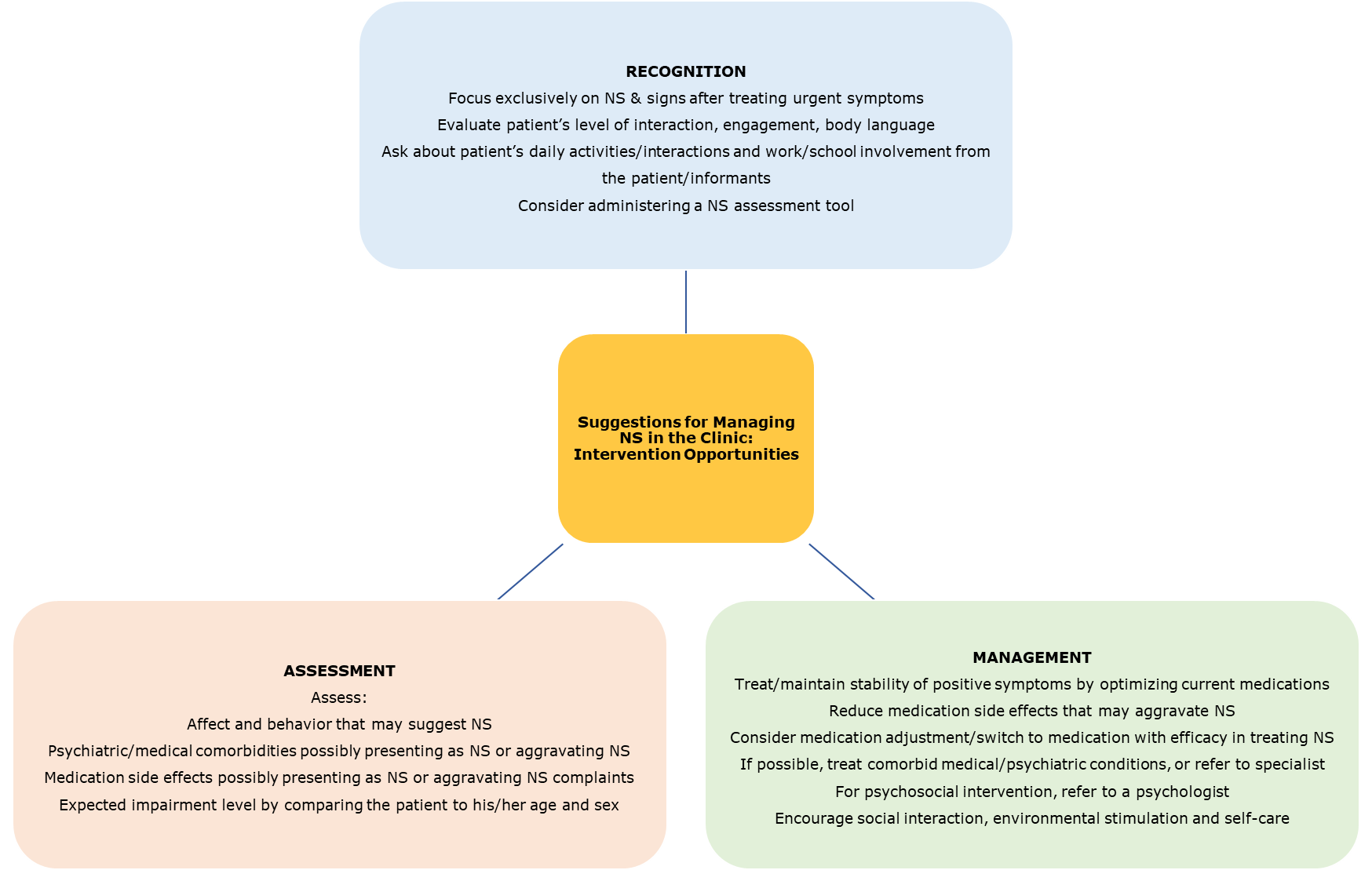
Even though the results from these psychosocial treatments are mixed and inconsistent, the article maintains that these may be an “important way for clinicians to support patients and their families as they cope with negative symptoms and attempt to improve outcomes and quality of life.” To help patients reach improved outcomes, negative symptoms need to be recognized, assessed and management as best as possible.
Negative symptoms occur in most schizophrenia patients and often remain unrecognized by clinicians. Even if recognized, there is only limited evidence-based treatment against negative symptoms, causing poor patient functionality, low productivity and a decline in quality of life. Monotherapy agents tested in well-designed clinical trials (i.e. cariprazine) have shown promise in improving negative symptoms.
References
- Correll et al. Negative symptoms in Schiophrenia: a review and clinical guide for recognition, assessment and treatment. Neuropsychiatric Disease and Treatment 2020:16 519–534
Neuropsychiatric Disease and Treatment
Negative Symptoms in Schizophrenia: A Review and Clinical Guide for Recognition, Assessment, and Treatment
CLOSER LOOK AT NEGATIVE SYMPTOMS!CLOSER LOOK AT NEGATIVE SYMPTOMS!
Negative symptoms are symptoms of loss or absence of normal function relating to motivation and interest, or emotional expression. Evidence does not support theNegative symptoms are symptoms of loss or absence of normal function relating to motivation and interest, or emotional expression. Evidence does not support the
more…REAGILA CONTROLS NEGATIVE SYMPTOMSOUR PRODUCT ON NEGATIVE SYMPTOMS
Negative symptoms of schizophrenia can occur as primary symptoms that are part of the underlying pathophysiology of schizophrenia or as secondary symptoms that Negative symptoms of schizophrenia can occur as primary symptoms that are part of the underlying pathophysiology of schizophrenia or as secondary symptoms that
more…