Switching to REAGILA
- In patients with acute symptoms or patients receiving high doses of previous antipsychotics, a faster titration with daily 1.5 mg dose increases may be preferable7-10.
- A gradual cross-titration has been shown to be safe and effective in patients with stable negative symptoms. These patients may be particularly good candidates for cariprazine, since cariprazine has proven greater improvement in this symptom domain compared to another antipsychotic4,5.
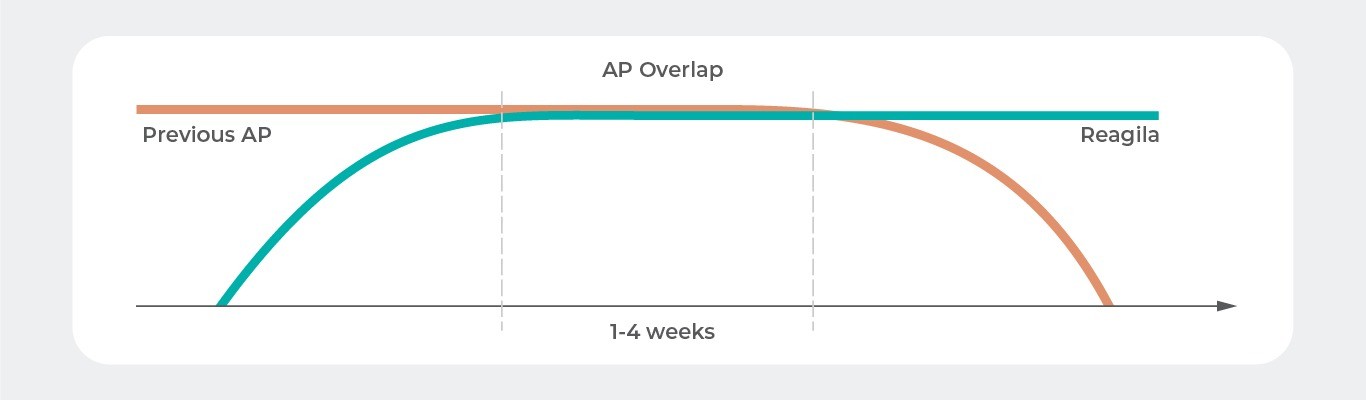
- A full-dose overlap period of a few weeks before dose de-escalation of the discontinued antipsychotic may also be appropriate when switching to a partial agonist like cariprazine10-12.
In this section
Why Would a Patient Switch Antipsychotic Treatment?
The ultimate goal in schizophrenia treatment is recovery, which encompasses symptom remission in addition to adequate self-care, improved social and vocational functioning, maintenance of treatment effects, and relapse prevention1. To achieve treatment success, an antipsychotic must reduce acute symptoms, and achieve response and remission with minimal and tolerable side effects so patients can adhere to their treatment regimen2. The decision to switch to another antipsychotic usually involves symptom-related issues or tolerability problems for stable patients. For example, residual symptoms, agitation, mood symptoms, continuing negative symptoms and cognitive dysfunction, lack of psychosocial or functional improvement, or impending relapse could precipitate a medication switch. In patients with stable disease, bothersome side effects such as weight gain, nausea, somnolence, or metabolic issues may warrant a switch to a different antipsychotic3.
Switching to Cariprazine
Clinicians may choose to switch from another antipsychotic to cariprazine15. Patients with persistent negative symptoms may be particularly good candidates since cariprazine has proven greater improvement in this symptom domain4,5 compared with other antipsychotics4,6,15.
Although different strategies can be employed when switching to cariprazine, a gradual cross-titration has been shown to be safe and effective in the cariprazine negative symptom study4,15. In this study, the patient’s current antipsychotic treatment remained unchanged in a 4-week prospective lead-in period. During the first part of double-blind treatment, a concurrent up-titration of cariprazine and down-titration of the prior antipsychotic occurred15. For this cross-titration, cariprazine was initiated at 1.5 mg/d for 6 days, followed by an increase to 3 mg/d on days 7 to 13, and then an increase to cariprazine 4.5 mg/d on day 1415. The prior antipsychotic, which was concurrently down-titrated to mirror the up-titration of cariprazine, was discontinued on day 1415. The down-titration process could be delayed for a maximum duration of 4 weeks if a risk of psychotic deterioration or withdrawal symptoms was anticipated4.
Cross-Titration When Switching to Cariprazine
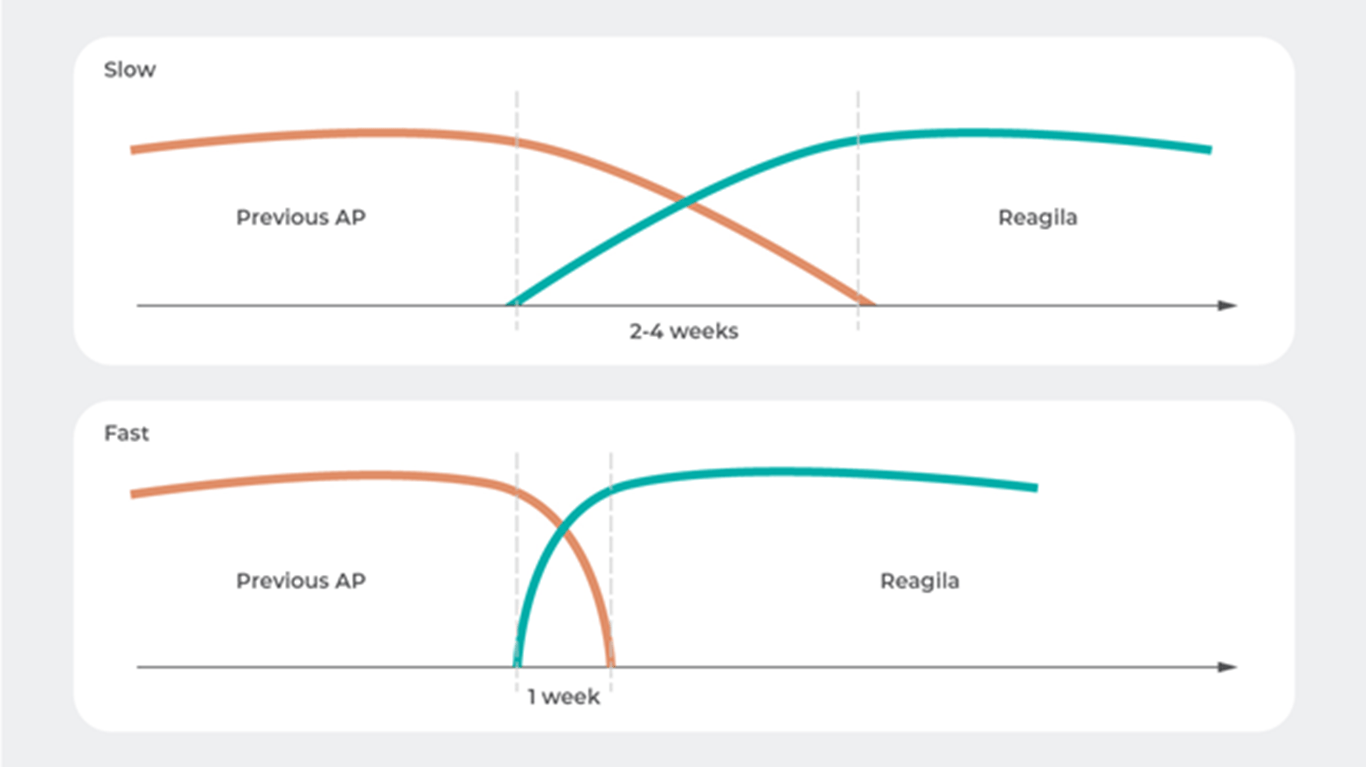
Although the safe and effective use of a slow up-titration strategy has been demonstrated in a population of patients with stable symptoms of schizophrenia in the negative symptom study4, other strategies for switching to cariprazine may be more appropriate in other situations3,15. For example, in patients with acute symptoms or patients receiving high doses of previous antipsychotics, a faster titration with daily 1.5 mg dose increases may be preferable7-10. Likewise, the optimal speed of down-titration of the previous antipsychotic may vary based on its half-life and anticipated risk of effects from dopamine receptor hypersensitivity or anticholinergic withdrawal syndrome3,10.
Patients With Stable Symptoms Can Undergo a Slow Titration Schedule, While Those With Acute Symptoms May Benefit From Faster Titration4,7-10
Reference: Adapted from Stahl, S. M. Stahl ’ s Essential Psychopharmacology: Prescriber’s Guide. Cambridge University Press. (2017)10
Down-Titration of Previous Agent When Switching to Cariprazine
When switching to cariprazine, the receptor profile of the antipsychotic you are switching from may influence the down-titration schedule15. Depending on the circumstances, various strategies may be appropriate, although knowledge of the pharmacokinetic/ pharmacodynamic principles of the drugs involved and expert clinical management are key3.
For switching to cariprazine, recommendations and guidance based on clinical data for switching from a currently administered antipsychotic to aripiprazole, a dopamine D2/D3 receptor partial agonist with relatively similar pharmacological characteristics to cariprazine, may provide supportive information15. A search of the literature was performed to identify recommendations and guidelines for switching to aripiprazole in the attempt to give a prototype example for cariprazine15.
Expert Consensus: A Prototype Example for Cariprazine
Two consensus papers were recently published that add valuable information to the literature about switching to aripiprazole. Panels of experts in psychiatry from Turkey (2018)11 and Italy (2015)12 each recommended up-titration of aripiprazole, a period of overlap with the previous antipsychotic for about 2 weeks, followed by de-escalation of the previous antipsychotic dose (5%-20% every 15 days depending on the previous antipsychotic). This full-dose overlap strategy is consistent with a strategy recommended by a 2007 multidisciplinary UK panel of experts13.
A Full-Dose Overlap Strategy is Often Recommended When Switching Between Antipsychotics11-13
Reference: Adapted from Veznedaroglu, B., Dilbaz, N., Uzun, O. & Isik, E. TARC: Turkish aripiprazole consensus report- Aripiprazole use and switching from other antipsychotics to aripiprazole- consensus recommendations by a Turkish multidisciplinary panel. Ther. Adv. Psychopharmacol. 8, 271–285 (2018)11
Switching From Antipsychotics That May Cause Problems
Sometimes switching to cariprazine may be complicated by the receptor profile of the antipsychotic that is being discontinued15. Awareness that switching from certain drugs may cause symptoms or side effects is important. Clinicians should use cross-titration strategies to minimize problems related to the drug that is being discontinued and give patients ample time to adjust to the drug that is being initiated3.
For example, if a patient is switching from a medication with strong antihistaminergic or anticholinergic properties (eg, clozapine, olanzapine or quetiapine), there is a possibility that upregulated and/or sensitized receptors could promote histaminergic or cholinergic activity10. In such cases, slower down-titration may reduce the risk of rebound symptoms (eg, agitation, insomnia, anxiety, restlessness, EPS, akathisia)3,10. Similarly, switching from a strong antidopaminergic medication, such as risperidone, haloperidol, or paliperidone, to a partial D2 agonist may result in psychosis or agitation, possibly due to hypersensitized and/or upregulated D2 receptors14. In cases like these, slower down-titration should also be considered. Further, discontinuing an agent with central muscarinic blockade may cause agitation, confusion, psychosis, insomnia, anxiety, and EPS/akathisia, while removal of serotonin receptor blockade may result in anxiety, EPS/akathisia and possibly psychosis and decreased appetite14.
A Personalized Switching Strategy May Be Best
Given all the relevant factors when switching from one antipsychotic to another, any overlap and tapering strategy should be personalized and adjusted to the individual patient and the individual antipsychotic agents involved3. Patient response and clinical history, including disease state, symptom severity, the receptor profile of previous agent, and the duration of treatment with the previous antipsychotic should all be considered3.
A gradual cross-titration strategy has been shown to be safe and effective for switching from another antipsychotic to cariprazine in a clinical trial in stable patients4,15. Similar to what has been recommended by expert consensus panels, however, a full-dose overlap period of a few weeks before dose de-escalation of the discontinued antipsychotic may also be appropriate when switching to a partial agonist like cariprazine11-13,15.
References
- Haller, C. S., Padmanabhan, J. L., Lizano, P., Torous, J. & Keshavan, M. Recent advances in understanding schizophrenia. F1000Prime Rep. 6, 1–11 (2014).
- Kahn, R. S. et al. Schizophrenia. Nat. Rev. Dis. Prim. 1, 1–23 (2015).
- National Health Institute Humber. Guidelines for Antipsychotic Medication Switches. (2000).
- Németh, G. et al. Cariprazine versus risperidone monotherapy for treatment of predominant negative symptoms in patients with schizophrenia: a randomised, double-blind, controlled trial. Lancet 389, 1103–1113 (2017).
- Fleischhacker, W. et al. The efficacy of cariprazine in negative symptoms of schizophrenia: Post hoc analyses of PANSS individual items and PANSS-derived factors. Eur. Psychiatry 58, 1–9 (2019).
- Earley, W. et al. Efficacy of cariprazine on negative symptoms in patients with acute schizophrenia: A post hoc analysis of pooled data. Schizophr. Res. 204, 282–288 (2019).
- Durgam, S. et al. An evaluation of the safety and efficacy of cariprazine in patients with acute exacerbation of schizophrenia: A phase II, randomized clinical trial. Schizophr. Res. 152, 450–457 (2014).
- Durgam, S. et al. Cariprazine in acute exacerbation of schizophrenia: A fixed-dose, phase 3, randomized, double-blind, placebo- and active-controlled trial. J. Clin. Psychiatry 76, e1574-82 (2015).
- Kane, J. M. et al. Efficacy and Safety of Cariprazine in Acute Exacerbation of Schizophrenia: Results from an International, Phase III Clinical Trial. J. Clin. Psychopharmacol. 35, 367–373 (2015).
- Stahl, S. M. Stahl ’ s Essential Psychopharmacology: Prescriber’s Guide. (Cambridge University Press, 2017).
- Veznedaroglu, B., Dilbaz, N., Uzun, O. & Isik, E. TARC: Turkish aripiprazole consensus report- Aripiprazole use and switching from other antipsychotics to aripiprazole- consensus recommendations by a Turkish multidisciplinary panel. Ther. Adv. Psychopharmacol. 8, 271–285 (2018).
- Fagiolini, A., Brugnoli, R., Di Sciascio, G., De Filippis, S. & Maina, G. Switching antipsychotic medication to aripiprazole: Position paper by a panel of Italian psychiatrists. Expert Opin. Pharmacother. 16, 727–737 (2015).
- Sullivan, G. et al. Practical prescribing with aripiprazole in schizophrenia: Consensus recommendations of a UK multidisciplinary panel. Curr. Med. Res. Opin. 23, 1733–1744 (2007).
- Correll, C. U. From receptor pharmacology to improved outcomes: Individualising the selection, dosing, and switching of antipsychotics. Eur. Psychiatry 25, S12-21 (2010).
- Reagila SmPC.
European Psychiatry
Correll CU. From receptor pharmacology to improved outcomes: individualising the selection, dosing, and switching of antipsychotics. Eur Psychiatry 2010;25(Suppl 2):S12-21.
STARTING DOSES FOR REAGILASTARTING DOSES FOR OUR PRODUCT
REAGILA is indicated for the treatment of schizophrenia in adult patients. This covers all types of symptoms of schizophrenia, including positive, negative, cogFind out more about the starting doses from first episode to relapse
more…REAGILA AND DRUG INTERACTIONSCARIPRAZINE AND DRUG INTERACTIONS
Cariprazine is metabolized into 2 pharmacologically active moieties: desmethyl cariprazine (DCAR) and didesmethyl cariprazine (DDCAR). This metabolism is mediatCariprazine is metabolized into 2 pharmacologically active moieties: desmethyl cariprazine (DCAR) and didesmethyl cariprazine (DDCAR). This metabolism is mediat
more…